Abstract
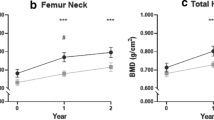
Parathyroid surgery is indicated in patients presenting with primary hyperparathyroidism (PHPT) and osteoporosis (defined as bone mineral density more than 2 standard deviations below normal). Many are elderly women with complex medical problems, either unwilling or considered unfit for surgery. Estrogen replacement therapy (ERT) may potentially be an alternative form of therapy in this group. We studied 15 consecutive postmenopausal women presenting with PHPT and osteoporosis. Group 1 comprised 5 women who elected to be treated with ERT (conjugated equine estrogen, 0.3–0.625 mg/day). The other 10 women underwent successful parathyroidectomy. These 10 patients were randomly subdivided into group 2 (5 patients who received calcitriol 0.25 µg b.i.d. for 12 months following surgery) and group 3 (5 patients who received elemental calcium 1 g/day for 12 months following surgery). Lumbar spine and femoral neck bone mineral density (BMD) were measured prior to and after 12 months of therapy, using a dual-energy X-ray absorptiometer (Lunar DPX-L). The three groups did not differ with respect to their ages (group mean 71.8 years), or baseline serum calcium (group mean 2.77 mmol/l), serum parathyroid hormone (group mean 11.0 pmol/l), lumbar spine BMD (group mean 0.93 g/cm2) and femoral neck BMD (group mean 0.73 g/cm2). Serum calcium normalized in all patients who underwent surgery and none developed hypoparathyroidism. A non-significant decrease in serum calcium was seen in patients treated with ERT only. Lumbar spine (+5.3% per year; 95% CI, 1.1% to 9.6%) and femoral neck BMD (+5.5% per year; 95% CI, −2.1% to 13.2%) increased significantly after 12 months of ERT (p<0.001 compared with pre-therapy values). These increases in BMD did not differ significantly from those in patients who underwent successful parathyroidectomy followed by either calcitriol therapy or calcium replacement (lumbar spine BMD increase of +6.2% per year, 95% CI 3.1% to 9.4%; and femoral neck BMD increase of +3% per year, 95% CI 0 to 6%). In summary, increases in lumbar spine and femoral neck BMD occur following treatment of PHPT. ERT appeared as effective as parathyroidectomy (combined with either calcitriol or calcium supplements) for the treatment of osteoporosis in elderly postmenopausal women presenting with PHPT.
Similar content being viewed by others
References
Genant HK, Heck LL, Lanzl LH, Rossman K, Horst JV, Paloyan E. Primary hyperparathyroidism: a comparative study of clinical, biochemical and radiological manifestations. Radiology 1973;109:513–24.
Lindsay R. Estrogen treatment of patients with established postmenopausal osteoporosis. Obstet Gynecol 1990;76:290–5.
Ettinger B, Genant HK, Cann CE. Postmenopausal bone loss is prevented by treatment with low-dosage estrogen with calcium. Ann Intern Med 1987;106:40–5.
Marcus R, Madvig P, Crim M, Pont A, Kosek J. Conjugated estrogens in the treatment of postmenopausal women with hyperparathyroidism. Ann Intern Med 1984;100:633–40.
Selby PL, Peacock M. Ethinyl estradiol and norethindrone in the treatment of primary hyperparathyroidism in postmenopausal women. N Engl J Med 1986;314:1481–5.
Marcus R. Estrogens and progestins in the management of primary hyperparathyroidism. J Bone Miner Res 1991;6:S 125–9.
McDermott MT, Perloff JJ, Kidd GS. Effects of mild asyptomatic primary hyperparathyroidism on bone mass in women with and without estrogen replacement therapy. J Bone Miner Res 1994;9:509–14.
Grey AB, Stapleton JP, Evans MC, Reid IR. A randomised, control trial of the effect of estrogen/progestin therapy on one mineral density in postmenopausal women with primary hyperparathyroidism [abstract]. J Bone Miner Res 1995;10:S 153.
Leppla DC, Snyder W, Pak CYC. Sequential changes in bone density before and after parathyroidectomy in primary hyperparathroidism. Invest Radiol 1982;17:604–6.
Mautalen C, Reyes HR, Ghiringhelli G, Fromm G. Cortical bone mineral content in primary hyperparathyroidism: changes after parathyroidectomy. Acta Endocrinol (Copenh) 1986;111:494–7.
Martin P, Bergmann P, Gillet C, et al. Partial reversible osteope-nia after surgery for primary hyperparathyroidism. Arch Intern Med 1986;146:689–91.
Silverberg SJ, Gartenberg F, Jacobs TP, et al. Increased bone mineral density after parathyroidectomy in primary hyperparathyroidism. J Clin Endocrinol Metab 1995;80:729–34.
National Institutes of Health. Consensus development conference statement on primary hyperparathyroidism. J Bone Miner Res 1991;6:S9–13.
Diamond T, McGuigan L, Barbagallo S, Bryant C. Cyclical etidronate plus ergocalciferol prevents glucocorticoid-induced bone loss in postmenopausal women. Am J Med 1995;98:459–63.
Silverberg SJ, Gartenberg F, Jacobs TP, et al. Longitudinal measurements of bone density and biochemical indices in untreated primary hyperparathyroidism. J Clin Endocrinol Metab 1995;80:723–8.
Marcus R. Bone of contention: the problem of mild hyperparathyroidism. J Clin Endocrinol Metab 1995;80:720–2.
Peacock M. Interpretation of bone mass determinations as they relate to fracture: implications for asymptomatic primary hyperparathyroidism. J Bone Miner Res 1991;6:S77–82.
Seeman E, Wahner HW, Offord KP, Kumar R, Johnson WJ, Riggs BL. Differential effects of endocrine dysfunction on the axial and appendicular skeleton. J Clin Invest 1982;69:1302–9.
Silverberg SJ, Shane E, De La Cruz L, et al. Skeletal disease in primary hyperparathyroidism. J Bone Miner Res 1989;4:283–91.
Gallagher JC, Wilkinson R. The effect of ethinyl estradiol on calcium and phosphorus metabolism of postmenopausal women with primary hyperparathyroidism. Clin Sci Mol Med 1973;45:785–802.
Cosman F, Shen V, Xie F, Seibel M, Ratcliffe A, Lindsay R. Estrogen protection against bone resorbing effects of parathyroid hormone infusion. Calcif Tissue Int 1993;118:337–43.
Manolagas SC, Jilka RL. Bone marrow, cytokines and bone remodelling. N Engl J Med 1995;332:305–11.
Girasole G, Jilka RL, Passed G, et al. 17β-estradiol inhibits interleukin-6 production by bone marrow-derived stromal cells and osteoblasts in vitro: a potential mechanism for anti-osteoporotic effect of estrogens. J Clin Invest 1992;89:883–91.
Brown EM, Pollak M, Seidman CE, et al. Calcium-ion-sensing cell-surface receptors. N Engl J Med 1995;333:234–40.
Eriksen EF, Mosekilde L, Melsen F. Trabecular bone remodeling and balance in primary hyperparathyroidism. Bone 1986;7:213–21.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Diamond, T., Ng, A.T.M., Levy, S. et al. Estrogen replacement may be an alternative to parathyroid surgery for the treatment of osteoporosis in elderly postmenopausal women presenting with primary hyperparathyroidism: A preliminary report. Osteoporosis Int 6, 329–333 (1996). https://doi.org/10.1007/BF01623394
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01623394