Abstract
Purpose
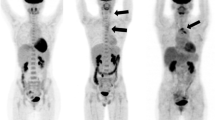
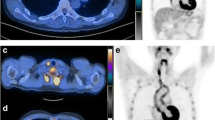
This study was performed to investigate the value of 18F-fluorodeoxyglucose positron emission tomography ([18F]FDG-PET) in the diagnosis of large-vessel vasculitis and the assessment of activity and extent of disease.
Methods
Twenty-six consecutive patients (21 females, 5 males; median age – years, range 17–86 years) with giant cell arteritis or Takayasu’s arteritis were examined with [18F]FDG-PET. Follow-up scans were performed in four patients. Twenty-six age- and gender-matched controls (21 females, 5 males; median age 71 years, range 17–86 years) were included. The severity of large-vessel [18F]FDG uptake was visually graded using a four-point scale. C-reactive protein (CRP) and the erythrocyte sedimentation rate (ESR) were measured and correlated with [18F]FDG-PET results by logistic regression.
Results
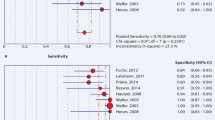
[18F]FDG-PET revealed pathological findings in 18 of 26 patients. Three scans were categorised as grade I, 12 as grade II and 3 as grade III arteritis. Visual grade was significantly correlated with both CRP and ESR levels (p=0.002 and 0.007 respectively; grade I: CRP 4.0 mg/l, ESR 6 mm/h; grade II: CRP 37 mg/l, ESR 46 mm/h; grade III: CRP 172 mg/l, ESR 90 mm/h). Overall sensitivity was 60% (95% CI 40.6–77.3%), specificity 99.8% (95% CI 89.1–100%), positive predictive value 99.7% (95% CI 77–100%), negative predictive value 67.9% (95% CI 49.8–80.9%) and accuracy 78.6% (95% CI 65.6–88.4%). In patients presenting with a CRP <12 mg/l or an ESR <12 mm/h, logistic regression revealed a sensitivity of less than 50%. In patients with high CRP/ESR levels, sensitivity was 95.5%/80.7%.
Conclusion
[18F]FDG-PET is highly effective in assessing the activity and the extent of large-vessel vasculitis. Visual grading was validated as representing the severity of inflammation. Its use is simple and provides high specificity, while high sensitivity is achieved by scanning in the state of active inflammation.





Similar content being viewed by others
References
Salvarani C, Silingardi M, Ghirarduzzi A, Lo Scocco G, Macchioni P, Bajocchi G, et al. Is duplex ultrasonography useful for the diagnosis of giant-cell arteritis? Ann Intern Med 2002;137:232–8.
Blockmans D. Utility of imaging studies in assessment of vascular inflammation. Cleve Clin J Med 2002;69 Suppl 2:SII95–9.
Tso E, Flamm SD, White RD, Schvartzman PR, Mascha E, Hoffman GS. Takayasu arteritis: utility and limitations of magnetic resonance imaging in diagnosis and treatment. Arthritis Rheum 2002;46:1634–42.
Kissin EY, Merkel PA. Diagnostic imaging in Takayasu arteritis. Curr Opin Rheumatol 2004;16:31–7.
Seo P, Stone JH. Large-vessel vasculitis. Arthritis Rheum 2004;51:128–39.
Ishimori T, Saga T, Mamede M, Kobayashi H, Higashi T, Nakamoto Y, et al. Increased 18F-FDG uptake in a model of inflammation: concanavalin A-mediated lymphocyte activation. J Nucl Med 2002;43:658–63.
Jones HA, Cadwallader KA, White JF, Uddin M, Peters AM, Chilvers ER. Dissociation between respiratory burst activity and deoxyglucose uptake in human neutrophil granulocytes: implications for interpretation of 18F-FDG PET images. J Nucl Med 2002;43:652–7.
Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum 1990;33:1122–8.
Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 1990;33:1129–34.
Moosig F, Czech N, Mehl C, Henze E, Zeuner RA, Kneba M, et al. Correlation between 18-fluorodeoxyglucose accumulation in large vessels and serological markers of inflammation in polymyalgia rheumatica: a quantitative PET study. Ann Rheum Dis 2004;63:870–3.
Turlakow A, Yeung HW, Pui J, Macapinlac H, Liebovitz E, Rusch V, et al. Fludeoxyglucose positron emission tomography in the diagnosis of giant cell arteritis. Arch Intern Med 2001;161:1003–7.
Blockmans D, Van Moer E, Dehem J, Feys C, Mortelmans L. Positron emission tomography can reveal abdominal periaortitis. Clin Nucl Med 2002;27:211–2.
Wenger M, Gasser R, Donnemiller E, Erler H, Glossmann H, Patsch JR, et al. Images in cardiovascular medicine. Generalized large vessel arteritis visualized by 18fluorodeoxyglucose-positron emission tomography. Circulation 2003;107:923.
Brodmann M, Lipp RW, Aigner R, Pilger E. Positron emission tomography reveals extended thoracic and abdominal peri-aortitis. Vasc Med 2003;8:127–8.
Wiest R, Gluck T, Schonberger J, Scholmerich J, Eilles C, Muller-Ladner U. Clinical image: occult large vessel vasculitis diagnosed by PET imaging. Rheumatol Int 2001;20:250.
De Winter F, Petrovic M, Van de Wiele C, Vogelaers D, Afschrift M, Dierckx RA. Imaging of giant cell arteritis: evidence of splenic involvement using FDG positron emission tomography. Clin Nucl Med 2000;25:633–4.
Hara M, Goodman PC, Leder RA. FDG-PET finding in early-phase Takayasu arteritis. J Comput Assist Tomogr 1999;23:16–8.
Malik IS, Harare O, AL-Nahhas, Beatt K, Mason J. Takayasu’s arteritis: management of left main stem stenosis. Heart 2003;89:e9.
Bleeker-Rovers CP, Bredie SJ, van der Meer JW, Corstens FH, Oyen WJ. Fluorine 18 fluorodeoxyglucose positron emission tomography in the diagnosis and follow-up of three patients with vasculitis. Am J Med 2004;116:50–3.
Blockmans D, Maes A, Stroobants S, Nuyts J, Bormans G, Knockaert D, et al. New arguments for a vasculitic nature of polymyalgia rheumatica using positron emission tomography. Rheumatology (Oxford) 1999;38:444–7.
Blockmans D, Stroobants S, Maes A, Mortelmans L. Positron emission tomography in giant cell arteritis and polymyalgia rheumatica: evidence for inflammation of the aortic arch. Am J Med 2000;108:246–9.
Webb M, Chambers A, AL-Nahhas A, Mason JC, Maudlin L, Rahman L, et al. The role of 18F-FDG PET in characterising disease activity in Takayasu arteritis. Eur J Nucl Med Mol Imaging 2004;31:627–34.
Meller J, Strutz F, Siefker U, Scheel A, Sahlmann CO, Lehmann K, et al. Early diagnosis and follow-up of aortitis with [18F]FDG PET and MRI. Eur J Nucl Med Mol Imaging 2003;30:730–6.
Rudd JH, Warburton EA, Fryer TD, Jones HA, Clark JC, Antoun N, et al. Imaging atherosclerotic plaque inflammation with [18F]-fluorodeoxyglucose positron emission tomography. Circulation 2002;105:2708–11.
Yun M, Yeh D, Araujo LI, Jang S, Newberg A, Alavi A. F-18 FDG uptake in the large arteries: a new observation. Clin Nucl Med 2001;26:314–9.
Yun M, Jang S, Cucchiara A, Newberg AB, Alavi A. 18F FDG uptake in the large arteries: a correlation study with the atherogenic risk factors. Semin Nucl Med 2002;32:70–6.
Kerr GS. Takayasu’s arteritis. Rheum Dis Clin North Am 1995;21:1041–58.
Evans JM, O’Fallon WM, Hunder GG. Increased incidence of aortic aneurysm and dissection in giant cell (temporal) arteritis. A population-based study. Ann Intern Med 1995;122:502–7.
Liu G, Shupak R, Chiu BK. Aortic dissection in giant-cell arteritis. Semin Arthritis Rheum 1995;25:160–71.
Greene GM, Lain D, Sherwin RM, Wilson JE, McManus BM. Giant cell arteritis of the legs. Clinical isolation of severe disease with gangrene and amputations. Am J Med 1986;81:727–33.
Nordborg E, Bengtsson BA. Death rates and causes of death in 284 consecutive patients with giant cell arteritis confirmed by biopsy. BMJ 1989;299:549–50.
Meller J, Grabbe E, Becker W, Vosshenrich R. Value of F-18 FDG hybrid camera PET and MRI in early takayasu aortitis. Eur Radiol 2003;13:400–5.
Belhocine T, Blockmans D, Hustinx R, Vandevivere J, Mortelmans L. Imaging of large vessel vasculitis with 18FDG PET: illusion or reality? A critical review of the literature data. Eur J Nucl Med Mol Imaging 2003;30:1305–13.
Brodmann M, Lipp RW, Passath A, Seinost G, Pabst E, Pilger E. The role of 2-18F-fluoro-2-deoxy-D-glucose positron emission tomography in the diagnosis of giant cell arteritis of the temporal arteries. Rheumatology (Oxford) 2004;43:241–2.
Acknowledgements
The authors are grateful to Drs. J. Baumann, H. Braun, H.J. Eglin, B. Frauchiger, S. Kneifel, H. Rasch and B. Trimpin for their support for this work. The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walter, M.A., Melzer, R.A., Schindler, C. et al. The value of [18F]FDG-PET in the diagnosis of large-vessel vasculitis and the assessment of activity and extent of disease. Eur J Nucl Med Mol Imaging 32, 674–681 (2005). https://doi.org/10.1007/s00259-004-1757-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-004-1757-9