Abstract
Approximately 30 % of colorectal carcinomas develop via the serrated neoplasia pathway characterized by widespread DNA methylation and frequent BRAF mutation. Serrated polyps represent a heterogeneous group of polyps which are the precursor lesions to serrated pathway colorectal carcinomas. The histological classification of serrated polyps has evolved over the last two decades to distinguish three separate entities: hyperplastic polyp, sessile serrated adenoma (SSA), and traditional serrated adenoma (TSA). The malignant potential of SSAs and TSAs has been clearly demonstrated. SSAs are more challenging to detect by colonoscopy and are likely to account for some interval carcinomas of the proximal colon. Serrated polyposis syndrome is now widely recognized as conferring a high risk of colorectal carcinoma although its cause remains elusive. The current understanding of the actual malignant potential of each serrated polyp subtype is still limited due to the lack of large-scale prospective studies. Patient management guidelines have been recently updated although high-level evidence to support them is still required.
Similar content being viewed by others
Introduction
Colorectal carcinoma (CRC) is one of the most common cancers worldwide. Virtually all CRCs originate from a precursor benign polyp, which makes this cancer potentially preventable by appropriate screening colonoscopy programs in patients at increased risk. Until approximately 1990, colorectal polyps were classified into two groups: adenomatous polyps (conventional adenomas) with a well-recognized potential for malignant transformation and hyperplastic (or ‘metaplastic’) polyps thought to have no risk of malignant transformation. While conventional adenomas are still considered to represent the precursor lesions of the majority of CRC, the group of polyps previously called ‘hyperplastic polyps’ has now been divided in various subtypes with respect to their morphologic appearance, molecular alterations, and risk of malignant transformation.
Over the last 20 years, our understanding of CRC pathogenesis has evolved from the concept of a single disease progressing through a sequence of morphologic and genetic alterations [1] to the concept of molecular heterogeneity and tumor uniqueness [2]. CRC is currently classified into subgroups of tumors which share similar molecular alterations in correlation with morphologic appearance and clinical features [3, 4]. Such classifications can become more and more complex as the number of classifiers increases to reach a complete set of characteristics that underlies the concept of a unique tumor arising in a unique individual. Therefore a meaningful classification should retain parameters with clinical consequences for patient management such as prevention, treatment, and surveillance. The nature of the precursor polyp is an essential classifier of CRC because each tumor is thought to develop from a unique benign polyp with its own set of morphologic and molecular characteristics. The heterogeneity of CRC translates to a certain extent into the multiplicity of precursor polyp subtypes that we have only recently started to understand. Conventional adenomas are the precursor lesions to CRCs developing via the traditional adenoma–carcinoma pathway characterized by chromosomal instability (except in patients with Lynch syndrome). Serrated polyps are the precursors of CRCs developing through the serrated neoplasia pathway characterized by BRAF mutation, CpG island methylator phenotype (CIMP), with or without microsatellite instability (MSI).
Serrated polyps represent a group of polyps with various recently recognized subtypes associated with different colonoscopic appearance, histology, molecular alteration, and risk of progression to malignancy: hyperplastic polyp (HP), sessile serrated adenoma (SSA), and traditional serrated adenoma (TSA). In this review, we will present our current knowledge about serrated polyps and the challenges that pathologists, gastroenterologists, and molecular biologists still face in understanding the clinical significance of these lesions for the patients.
Prevalence and risk factors for serrated polyps
The prevalence of serrated polyps in the general population has been evaluated in autopsy studies to range from 13 to 40 % [5, 6]. In a prospective population-based colonoscopy study, Forsberg et al. [7] reported that 21 % of asymptomatic individuals had at least one hyperplastic polyp identified by colonoscopy. Studies of the prevalence and clinical features of serrated polyp subtypes are only meaningful if they were conducted after about 2005 when the entity of SSA was established and started to be recognized in the pathology community [8]. Prior to that time, most serrated polyps were considered to be HPs and epidemiological studies have limited utility in light of current knowledge. The prevalence of SSAs and TSAs in patients undergoing colonoscopy appears to be influenced by the patient population, endoscopy technique, and pathologic interpretation (Table 1). The true prevalence in different populations will become established as endoscopic detection and pathologic interpretation of these lesions become more standardized. In all series, SSAs were approximately ten times more common than TSAs.
The risk factors for SSAs and TSAs are still being defined. There is strong evidence from case control studies that smoking is associated with an increased risk of SSAs with an odds ratio of approximately 7 [9, 10]. This is supported by data showing an association between smoking and CRCs which are CIMP-high (high level of CIMP) and harbor BRAF mutation [11]. There is also strong evidence that there is a genetic predisposition to serrated neoplasia and that the genes involved may be more common in Caucasians [12, 13]. The genetic predisposition may be a continuum involving a number of genes, each of moderate effect, which interact with environmental factors such as smoking. At one end of the spectrum may be serrated polyposis whilst other individuals may have a few SSAs in the proximal colon and an increased lifetime risk of CIMP-high BRAF-mutated CRC [14, 15]. A recent population-based study showed an increased cancer predisposition in family members of patients with BRAF-mutated CRC [16]. There is likely to be overlap between the environmental and genetic risk factors for SSAs and conventional adenomas as individuals with SSAs are more likely to also have conventional adenomas as well as multiple serrated polyps [17–19].
Definition and histological classification of serrated polyps
In contrast to conventional adenomas, serrated polyps have in common a ‘saw-tooth’ appearance of the colonic crypts. This pattern is thought to result from decreased apoptosis and increased senescence of epithelial cells along the crypts [20]. According to the latest World Health Organization (WHO) classification published in 2010 [21], serrated polyps are now categorized into three main subtypes: hyperplastic polyps, sessile serrated adenoma/polyps without or with cytological dysplasia, and traditional serrated adenomas. The terms sessile serrated adenoma and sessile serrated polyp are both synonyms and acceptable in diagnostic use. An easy conceptual way to define and differentiate these subgroups is based on differences in location of the proliferation zones within the serrated crypts in each subgroup [22, 23]. In HP, the expanded proliferation zone is located at the base of the crypts (like in normal crypts) and cells mature towards the surface symmetrically. In SSA, the proliferation zone is shifted from the base to the side of the crypts resulting in maturation of epithelial cells towards the surface and the base, leading to crypt base dilatation. In TSA, the proliferation zone is represented by multiple small ectopic crypt formations from the side of the original crypts and along the newly formed villous projections of the polyp [23].
The main features defining each serrated polyp subtype are reported in Table 2 and Fig. 1. HPs are further subdivided into microvesicular HP and goblet cell HP. However, this distinction is mostly of academic interest at the present time and is usually not reported by pathologists. HPs represent the most innocuous subtype of serrated polyps but there are still unresolved questions on their possible evolution to more advanced polyps. It is unclear whether some microvesicular HP can progress to SSA or whether SSA can arise ab initio without an initial step of microvesicular HP. With the high prevalence of diminutive (≤5 mm) microvesicular HP found in the distal colorectum contrasting with the rarity of CRC with features of serrated neoplasia pathway diagnosed in this location, it is unlikely that distally located HPs have any malignant potential. Moreover, the significance of goblet cell HP is poorly understood; some authors have suggested that it may represent the precursor lesion of TSA [24, 25]. SSA is defined by a sessile polyp with abnormal crypt architecture and abnormal proliferation but no dysplasia. However, dysplasia can arise in SSA and usually appears as a sharply demarcated area of the polyp with cytological dysplasia resembling conventional adenoma. These polyps were often reported as mixed polyps in the past.
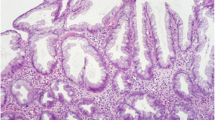
Histological appearances of various subtypes of serrated polyps. Hyperplastic polyps (a, b) are characterized by elongated crypts with overall preserved architecture. The serrated (‘saw-tooth’) appearance is on the upper part of the crypts with narrow bases. Note that the serration is more subtle in goblet cell hyperplastic polyps (b) compared to microvesicular hyperplastic polyps (a). Sessile serrated adenomas (c, d) demonstrate abnormal crypt architecture with broad bases and dilation of the crypts due to the shift of the proliferation zones from the base to the side of the crypts. Note the abundant mucus on the surface and in the crypt lumens corresponding to the mucus cap at colonoscopy. Sessile serrated adenoma can develop cytological dysplasia (right part of e) with complex crypt architecture and cytological atypia. Traditional serrated adenomas (f) are commonly exophytic polyps displaying villous projections with ectopic crypt formations and lined by cells with eosinophilic cytoplasm
With the advent of this new nomenclature, prior terminologies such as ‘serrated adenoma’, ‘variant HP’, or ‘mixed polyp’ should no longer be used. In most cases, pathologists are able to classify serrated polyps in each of these categories. However, there are a few situations whereby a definite histological diagnosis can be difficult to achieve. This can be secondary to an unusual appearance of a polyp that displays features of more than one polyp subtype. In this regard, the 2010 WHO classification definition states that if as few as two or three contiguous crypts demonstrate features of SSA in an otherwise HP-appearing polyp, the polyp should be classified as an SSA. Moreover, if a polyp displays an overall growth pattern of a TSA with ectopic crypt formations, but with a predominance of goblet cells (as opposed to tall eosinophilic cells with pencillate nuclei), the polyp should be classified as TSA. It should be noted that these definition criteria are based on a low level of biological evidence. Confusion also occurs when a polyp with an overall growth pattern of SSA displays cytologic features of TSA. A descriptive report is recommended until a better understanding of these lesions is known. Another common difficult situation arises when the polyp is obliquely sectioned, not showing the crypt bases to be able to distinguish HP from SSA. If deeper sections do not help, a diagnosis of ‘non-dysplastic serrated polyp, unclassified’ is recommended. Finally, it may be impossible for the pathologist to distinguish between piecemeal resection of an SSA with cytological dysplasia and the co-occurrence of separate conventional adenoma and SSA when information on the number of polyps submitted in one specimen bottle is lacking. Communication with the gastroenterologist should resolve this problem.
The issue of interobserver reproducibility among pathologists (including gastrointestinal pathologists) to diagnose SSA has been addressed by several groups, showing poor to moderate kappa values (0.14–0.55 between SSA and other polyps) [26–30]. It is anticipated that an increase in awareness among the pathology community and the release of the 2010 WHO criteria [21] will result in improvement of the reproducibility of serrated polyp diagnosis [31].
Molecular features of serrated polyps
Molecular data has complemented the evolution of serrated polyp nomenclature (Fig. 2). The most characteristic and well-studied molecular changes in serrated polyps are the mitogen activated protein kinase (MAPK) pathway activation through mutation of the BRAF oncogene and development of the CIMP. The importance of increased Wnt pathway signaling in serrated lesions has been debated, but may be important at the transition to dysplasia. Disruption of TP53 may also be involved in the progression of serrated polyps. Current challenges are to determine why BRAF is almost exclusively mutated in serrated polyps, whether this mutation directs polyp architecture, and whether it is sufficient to initiate polyp growth. A further challenge is to better understand the timing and targets of the CIMP, including which genes become methylated during polyp initiation versus progression.
Pathways of serrated neoplasia. Oncogenic BRAF mutation is detected in the earliest serrated lesions. Methylation changes are also established early in serrated polyp development, although frank CpG island methylator phenotype (CIMP) using highly specific markers may not be evident until the sessile serrated adenoma stage. Wnt pathway deregulation is more common in serrated polyps with cytological dysplasia, as is MLH1 DNA methylation which leads to microsatellite instability (MSI) and repeat tract mutation in genes such as TGFβRII. The TP53 gene is more commonly mutated in microsatellite stable (MSS) CRCs. Progression to either MSS or MSI CRC may occur through a traditional serrated adenoma intermediate (dashed arrows), although this is less common and not well documented. Progression to traditional serrated adenoma from goblet cell hyperplastic polyp or from conventional adenoma (dashed arrows) has also been hypothesized but not well studied
MAPK pathway activation
The MAPK signaling pathway is commonly altered in CRC and precursor lesions through oncogenic mutation of either the BRAF or KRAS genes. These mutations are mutually exclusive and demonstrate a striking specificity for serrated polyp subtype [19, 32, 33]. BRAF is mutated with increasing frequency in serrated aberrant crypt foci (62 %) [34], microvesicular HP (70–76 %) [19, 35], borderline SSA (80 %) [36], SSA (61–100 %) [19, 36–40], and SSA with cytological dysplasia or invasive cancer (64–100 %) [40, 41], supporting the concept of a histologic continuum. BRAF is uncommonly mutated in goblet cell HP. Rather, KRAS is mutated in approximately 50 % of goblet cell HP but rarely in microvesicular HP or SSA [19].
MAPK pathway activation is also common in TSA, but the relative proportion of BRAF versus KRAS mutation varies widely in different studies, probably reflecting differences in histological classification or small sample size. BRAF mutation rates in TSA range from 27 to 55 % [25, 42, 43] compared to 29–46 % for KRAS mutation [25, 42]. Refinement of the histological features of TSA will increase the consistency of diagnosis and therefore will clarify the involvement of the MAPK pathway in this uncommon polyp subtype.
CpG island methylator phenotype
The CpG island methylator phenotype (CIMP) describes the coordinate hypermethylation of multiple CpG dinucleotide clusters called CpG islands. These CpG islands often reside in gene promoter regions where aberrant DNA hypermethylation frequently correlates with silencing of the downstream gene. The phenotype targets many hundreds of CpG islands; however, the specific gene promoters involved and whether the associated genes become silenced and play a role in the serrated pathway require further investigation.
In CRC, CIMP is highly correlated with BRAF mutation. Rates of CIMP in serrated polyps vary depending on the marker panel used to identify the phenotype, but usually segregate with BRAF mutation. CIMP has been reported in 47–73 % of microvesicular HP, 70–76 % of SSA, and 80 % of SSA with cytological dysplasia [35, 44], suggesting that high levels of aberrant DNA methylation are established early in the serrated pathway. In fact, specific DNA methylation events have even been detected in histologically normal colorectal mucosa and this correlated with the presence of serrated polyps elsewhere in the bowel [45]. CIMP has been less well studied in TSA, but may occur in up to 79 % of cases [35]. TSA with a KRAS mutation may have lower rates of CIMP compared to those with a BRAF mutation, but this requires further investigation.
Other than specific CIMP panel markers, many hundreds of other gene promoters become hypermethylated in serrated polyps as part of this phenotype. Dhir et al. [46] recently showed accumulation of methylation events with progression of serrated lesions. An average methylation score was determined on the basis of 17 non-CIMP gene promoters which increased from HP to SSA, with highest scores in SSA with cytological dysplasia. The MLH1, CDX2, and TLR2 genes were specifically methylated in SSA and SSA with cytological dysplasia, but not in HP or conventional adenomas. MLH1 silencing is important for progression of a proportion of serrated polyps to cancers showing microsatellite instability. The p16 gene is a cell cycle inhibitor. Methylation-induced silencing of p16 allows escape from BRAF-induced senescence and also occurs with increasing frequency with neoplastic progression [47].
Wnt signaling pathway
The Wnt signaling pathway plays an important role in the initiation of conventional adenomas, usually through mutation and deletion of the APC tumor suppressor gene. A potential role in the progression of serrated polyps is more controversial. Wnt is a ligand that binds frizzled receptors on the cell membrane, which then signals to stabilize the APC–Axin–GSK3β degradation complex. When APC is silenced, the transcription factor β-catenin is no longer degraded by this complex, but rather accumulates in the cell nucleus, complexing with Tcf/lef to activate transcription of downstream targets that promote oncogenesis. Immunohistochemistry for β-catenin can be used to indicate alteration of Wnt signaling. The normal staining pattern in colonocytes is membranous, compared to nuclear when β-catenin is abnormally stabilized. Altered immunostaining is seen with increasing frequency with serrated polyp progression, although wide variability has been reported [40, 41, 48–56]. Interpretation of staining pattern including the proportion of cells involved and robust experimental methodology are critical to understanding the role of Wnt signaling in serrated polyps.
The Wnt signal may also be altered by genetic or epigenetic targeting of other genes in the signaling pathway. Integration of whole exome mutation and whole genome copy number and gene expression data suggested over 90 % of BRAF mutant tumors have altered Wnt signal, supporting a critical role in serrated as well as conventional neoplasia [57]. The role of Wnt signaling in serrated polyps may be further explored by examining genes in the pathway that may be silenced by DNA hypermethylation. For example, the Wnt pathway antagonists SFRP (types 1–5) are commonly methylated in SSA and SSA with dysplasia, but not in HP [46]. CDX2 is a transcription factor involved in epithelial cell proliferation and differentiation that inhibits the Wnt signal by binding β-catenin and disrupting the β-catenin–TCF complex [58]. The CDX2 gene promoter is methylated in SSA but not in HP or conventional adenomas [46]. MCC is another Wnt pathway molecule that directly interacts with β-catenin to dampen the Wnt signal and this is also methylated in HP and SSA but uncommonly in conventional adenomas [59].
p53 pathway alterations
The p53 tumor suppressor regulates cellular response to stress through the cell cycle and apoptosis. Aberrant nuclear accumulation of p53, which is suggestive of gene mutation, correlates with dysplastic changes in a proportion of SSAs and TSAs [41, 42]. Although no aberrant staining was observed in 66 HPs or 53 SSAs, 6/12 SSAs with a focus of dysplasia or cancer showed nuclear p53 accumulation [41]. Furthermore, in these and another series of 6/24 TSAs showing aberrant staining, p53 accumulation was limited to the dysplastic cells [41, 42]. Mutation of p53 is uncommon in the serrated neoplasia pathway cancers showing BRAF mutation, CIMP, and microsatellite instability, but is commonly mutated in the 50 % of BRAF mutant, CIMP-positive cancers that do not methylate MLH1 and are therefore microsatellite stable. It is possible that MLH1 methylation and p53 mutation are critical alterations leading to neoplastic change and transition to either microsatellite unstable or microsatellite stable CRC, respectively. IGFBP7 functions downstream of p53 to mediate its tumor suppressor function [60]. In serrated polyps that do not mutate p53, methylation of IGFBP7 may be an alternate mechanism for inactivating the p53 pathway. Interestingly, Kaji et al. [38] recently suggested that whilst MLH1 and IGFBP7 methylation may often coexist in serrated polyps, the order of events might be important for directing the neoplastic pathway. They hypothesized that primary methylation of IGFBP7 would result in TSA-like histology compared to SSA-like histology when MLH1 is methylated first.
Colonoscopic detection
Colonoscopic appearance
At colonoscopy, serrated lesions have a distinctive and characteristic appearance. Hyperplastic polyps are the most common serrated polyp subtype and are typically diminutive and located in the distal colon and rectum [19]. They are characteristically pale and flat or sessile, often with a translucent appearance such that they can be less visible with insufflation [61]. SSAs, which are typically larger than HPs and located in the proximal colon, are flat or non-polypoid in morphology [62], often with the appearance of redundant or thickened mucosa altering the contour of a fold, or appearing to be draped over a fold (Fig. 3) [63, 64]. A distinctive feature of SSAs is the mucus cap, comprising a layer of mucus adherent to the surface of the lesion, giving the lesion a yellow or rust-colored appearance in contrast to the surrounding mucosa [65]. The mucus cap assists in delineating the lesion from surrounding mucosa, such that when removed with mucosal irrigation, the edges of the lesion are indistinct and difficult to distinguish from surrounding normal mucosa. These characteristics were confirmed in a recent prospective study of 158 SSAs in which dominant features included a mucus cap, a rim of bubbles or debris, alteration of the contour of a fold, and loss of the normal mucosal vascular pattern (Table 3). TSA are typically located distally, are more bulky, and tend to be pedunculated or sessile [64].
Lesion characterization
Serrated lesions can be accurately and reliably distinguished from conventional adenomas during colonoscopy, using real-time image-enhancement technologies that are available on all current endoscopic platforms [66]. One such technology is narrow-band imaging (NBI), which utilizes a narrowed wavelength of light to highlight mucosal microvasculature. A recently validated international classification [67] for using NBI to determine real-time histology indicates that serrated lesions appear the same color or lighter than surrounding mucosa, have no blood vessels or only isolated lacy blood vessels coursing across the surface, and have no surface pattern or have dark or white spots of uniform size (Fig. 4).
Colonoscopic appearances of two sessile polyps with and without image enhancement: sessile serrated adenoma with high definition white light (a), NBI (narrow band imaging, Evis Exera II, Olympus Medical Systems Corporation, Japan) (b), and indigocarmine dyespray chromocolonoscopy (c); sessile serrated adenoma with white light (d), NBI (e), and with NBI after removal of mucus cap (f)
Real-time determination of serrated lesion subtype (SSA vs. HP vs. TSA) based on mucosal and morphological characteristics is limited, likely because the primary histological characteristics of SSAs are located in the base of the crypts [68]. Recent studies using optical magnification colonoscopy (which is not widely available in Western countries) have attempted to define endoscopic characteristics of SSAs, to allow real-time differentiation [64, 69, 70]. Kimura et al. [69] found that a modification to the Kudo pit-pattern classification, a novel type II-O (open) pit-pattern was specific, but not sensitive for SSAs. However, Hasegawa et al. [64] found discrimination difficult and instead relied on size and location of lesions. Furthermore, areas of dysplasia within an SSA may theoretically be distinguishable at colonoscopy, particularly with image enhancement techniques and/or optical magnification (Fig. 5); however, this has not been studied.
Colonoscopic detection
Colonoscopy is not a perfect test, and multiple factors contribute to the variable effectiveness of colonoscopy and its possible limitations for lesion detection. These include patient, technical, health system, and endoscopist factors, such as adequacy of bowel preparation, equipment or reimbursement incentives, and variation in the motivation, visuoperceptual capacity, and skills of the endoscopist [71, 72].
In particular, colonoscopy is less effective at preventing CRC in the proximal compared with the distal colon [73–78]. It is hypothesized that this in part relates to failures to detect, recognize, and completely resect SSA [79, 80]. Consistent with this hypothesis are data showing that cancers occurring after colonoscopy are more likely to be MSI-high and CIMP-high [81, 82], suggesting that they originated in unrecognized SSAs and that exposure to colonoscopy is associated with a lower risk of metachronous advanced conventional adenomas in both the proximal and distal colon, but not SSAs [79].
Failures in detection and recognition of SSAs therefore pose a major limitation of colonoscopy for CRC prevention. In fact, variation in the detection of serrated polyps between endoscopists is more substantial than the variation in endoscopist detection of conventional adenomas [83, 84]. Two studies now indicate the extent of this variation and suggest that miss rates for serrated polyps are far higher than for conventional adenomas. Specifically, Hetzel et al. [83] analyzed 4,335 polyps from 7,192 average-risk screening colonoscopies and found that proximal colon SSA prevalence varied between endoscopists from 0 to 1.4 %. The prevalence of SSAs also increased over time, from 0.2 % in 2006 to 1.1 % in 2008. Likewise, Kahi et al. [84] found in 6,681 colonoscopies that proximal serrated polyp prevalence (per colonoscopy) ranged between endoscopists from 1 to 26 %. As noted earlier, this variation has implications for understanding the true prevalence of SSA at colonoscopy.
Detection of serrated lesions is clearly operator-dependent, indicating that specific knowledge and skills are required for their detection and recognition. Lesion recognition requires “target familiarity” with their characteristic appearance, enabling the examiner to visually distinguish the lesion from the background normal mucosa [85]. It is likely that this requires extensive exposure to serrated lesion appearances [65] and repeated, deliberate clinical practice.
The role of specific colonoscopic technologies for improving the detection of serrated lesions is unclear. Studies of technologies to improve mucosal exposure at colonoscopy (e.g., cap-fitted colonoscopy [86], proximal colon retroflexion [87], and to improve recognition of subtle lesions, e.g., high definition colonoscopy [88], electronic image-enhancement [89], dyespray chromoendoscopy [90]) have not been specifically performed for serrated lesion targets [19]. In the largest study of pancolonic chromocolonoscopy with indigocarmine dyespray, Pohl et al. [91] found a significant increase in serrated lesion detection (1.19 vs. 0.49 per patient). It is likely that any beneficial impact of these technologies on serrated polyp detection will be greater for those endoscopists with lower baseline levels of polyp detection.
Management of patients with serrated polyps
Colonoscopic resection
Consensus recommendations are that all serrated lesions should be removed at colonoscopy, except for diminutive rectosigmoid hyperplastic polyps, which should be randomly sampled for histology [68, 92]. Optimal resection techniques are yet to be defined for serrated lesions, although specific challenges relate to their morphology and indistinct margins [93]. Cold snaring techniques (without electrocautery) are generally recommended for lesions under 10 mm [68, 94]. For larger lesions, electrocautery with or without submucosal injection is warranted. Image-enhancement techniques including NBI, topical dyespray application, or submucosal dye injection (e.g., indigocarmine) may assist in delineating the margin of the lesion. Early colonoscopic follow-up (at 3–6 months) is warranted for piecemeal resection of larger serrated lesions given the specific risks of incomplete resection with these lesions [95] and reports of early interval cancer [96].
Surveillance
Management of SSAs and TSAs depends on understanding their natural history particularly the transition to malignancy. There is abundant evidence that these lesions are associated with CRC [80, 97]. Perhaps more informative are studies of lesions “caught in the act” of transition to malignancy (Fig. 5). As discussed above, histological studies indicate an abrupt transition from SSA to SSA with high-grade cytological dysplasia and invasive malignancy and there is a case report of this transition occurring in an 8-month time period [98]. Three published case series show that the mean size of such lesions is not much greater than the mean size of typical SSAs without cytological dysplasia (Table 4).
Another study looked specifically at the median age of patients with SSAs and found it to be 61 years for SSA, 72 years for SSAs with high-grade dysplasia, and 76 years for patients presenting clinically with cancer related to an SSA [99]. Furthermore, females were over-represented amongst those patients with SSA progressing to high-grade dysplasia and malignancy. Overall, these data suggest that SSA may be present for many years with little change. However, in the cases where invasive malignancy does develop, this happens suddenly without a reliable window of warning signs such as low-grade dysplasia or polyp size greater than 10 mm. This interpretation of the data was also endorsed in recent consensus reviews [68, 92]. It would be very helpful if molecular or clinical markers able to predict which SSAs are most at risk of progression could be developed.
So far there is limited evidence on which to base recommendations for surveillance in patients found to have serrated polyps. In a group of 40 patients who had “hyperplastic polyps” removed between 1980 and 2001 whose polyps were SSAs on review and who were followed up for a mean of 13.2 years, five developed subsequent cancers and one had adenoma with high-grade dysplasia [100]. At the time of the detection of the SSA, these patients had no history of adenomas or cancer and so would not have been recommended to have surveillance according to the guidelines at the time. In another study, 39 patients were identified on colonoscopy between 1994 and 1997 as having proximal non-dysplastic serrated polyps as the only lesion in their bowel and underwent further colonoscopy within 5.5 years [97]. These patients had a 3.14-fold increased risk of adenoma during follow-up compared to control patients with no polyps.
A more recent study reported on 22 patients found to have at least one SSA at colonoscopy in 2005 [101]. Many but not all of these patients had synchronous adenomas or a history of prior polyps. Follow-up colonoscopy over the next 5 years found new SSAs in 11 (50 %) of these patients. Two of the SSAs displayed low-grade dysplasia and one high-grade dysplasia. Adenomas were found in 45 % of patients and one patient developed CRC. Another study published in 2012 reported 43 patients with at least one SSA diagnosed on colonoscopy between 2002 and 2004 with follow-up colonoscopy [102]. At an average of 2.72 years after the initial colonoscopy, SSAs were found in 22 patients (51 %), adenomas in 16 patients (37 %), SSA with high-grade dysplasia in 1 patient, and mucinous carcinoma developed in 1 patient.
Colonoscopy is an excellent tool to prevent CRC but it is costly, invasive, and carries some risk. Thus surveillance colonoscopy in patients known to be at risk aims to be frequent enough to detect lesions prior to malignant transformation but not unnecessarily frequent. To date, most national guidelines for colonoscopy surveillance after polypectomy agree that patients with small, distally located hyperplastic polyps do not require subsequent surveillance [68, 92, 103]. They recognized that other serrated lesions are significant but note that there is limited evidence to make firm recommendations.
Factors which may guide surveillance intervals include:
-
Histologic subtype: SSA and TSA are certainly predictive of a higher risk than HPs. It is likely that the presence of low-grade or high-grade cytological dysplasia in a SSA or TSA further heightens the risk of subsequent significant lesions.
-
Number of polyps: Almost certainly the risk of subsequent polyps and cancer increases with the number of polyps and the most extreme example of this is serrated polyposis where it is agreed that the surveillance interval should be 1 year [68].
-
Concomitant conventional adenomas: There is no direct evidence but it is likely that patients with a higher polyp burden due to the presence of both adenomas and serrated polyps are at greater risk.
-
Location in the colon: Most cancers arising in serrated polyps do so in the proximal colon. However most SSAs are themselves in the proximal colon and it is not certain whether the uncommon SSAs occurring in the distal colon are individually of less risk.
-
Size of polyps: It is likely that there is an increased risk in patients with larger SSAs but it is not clear that the cutoff of 10 mm used to define advanced conventional adenomas applies to SSAs. SSAs rarely grow larger than 20 mm [104] and most large polyps are adenomas. As discussed above, the average size of SSAs shown to contain invasive malignancy ranged from 8 to 11 mm.
The recently published guidelines shown in Table 5 were based on consensus expert opinion [68]. They are based on the premise that the colonoscopy is of good quality with a high detection rate of serrated lesions and that all serrated lesions are fully resected except for the most diminutive hyperplastic polyps in the distal bowel. They are also based on the premise that pathological interpretation of the lesions is consistent with the current WHO guidelines as described above. If there is doubt about the latter, a conservative position is to consider all proximal serrated lesions larger than 10 mm as SSAs even if they are reported as HPs [105]. These guidelines were endorsed in a simplified form in the 2012 American Gastroenterological Association guidelines for colonoscopy surveillance after screening and polypectomy [92]. It is recommended that patients with SSAs smaller than 10 mm and without dysplasia be followed up at 5 years and patients with TSAs or SSAs of at least 10 mm or with dysplasia be followed up at 3 years.
Serrated polyposis
Serrated polyposis syndrome (SPS) is the WHO’s preferred terminology for the condition previously called hyperplastic polyposis. The term SPS emphasizes the common occurrence of sessile serrated adenoma. Patients fulfilling one or more of the current following criteria are diagnosed with SPS: (1) at least five serrated polyps proximal to the sigmoid colon with two or more of these being larger than 10 mm; (2) any number of serrated polyps proximal to the sigmoid colon in an individual who had a first-degree relative with SP; (3) more than 20 serrated polyps of any size but distributed throughout the colon [21]. In practice, criterion 2 is rarely used. The number of polyps is cumulative over time. There has been recent interest in this syndrome with studies emphasizing the lack of awareness and the under-recognition of SPS among gastroenterologists and pathologists [106–109]. SPS is characterized by a continuum of phenotypes with polyposis commonly affecting the entire large bowel and the frequent co-occurrence of conventional adenoma (Fig. 6) [110]. The prevalence of SPS may be as high as 1/151 patients undergoing colonoscopy after positive fecal occult blood test [106]. Patients with SPS are at increased risk for CRC with the actual risk yet to be defined from prospective studies [111]. First-degree relatives are also at increased risk of CRC [112, 113], justifying the recommendation for screening colonoscopy in first-degree relatives aged at least 40 years or aged 10 years younger than the age of diagnosis of the youngest relatives [68, 114]. Further colonoscopy is recommended at 5-year intervals or more frequently if polyps are detected. The recommended colonoscopy surveillance interval in SPS patients is yearly with the aim to remove all polyps over 5 mm in size. Surgery is indicated when CRC is diagnosed or when a high polyp burden cannot be controlled by colonoscopy. Until a genetic hallmark of SPS is identified, the criteria for the diagnosis and the surveillance of this syndrome remain rather arbitrary.
Conclusions and perspectives
Serrated polyps comprise a diverse group of polyps with common morphological serrated appearance and distinct endoscopic, histological, and molecular profiles. There is growing evidence that interval CRCs in the proximal colon are caused by serrated polyps missed at colonoscopy. This represents a challenge for gastroenterologists to improve the detection rate of sessile polyps, many of which will be SSAs, by increased awareness and the use of advanced imaging techniques. Likewise pathologists should become more familiar with the histological features that distinguish SSA from HP and should use the WHO criteria to correctly diagnose serrated polyp subtypes. Because interobserver variability in histological diagnosis still exists, many experts consider that all serrated polyps in the proximal colon larger than 10 mm in size are likely to be SSAs, even if pathologists interpret them as HPs. The rarer lesion of TSA is still poorly understood and requires additional studies to refine criteria for diagnosis and understanding of the molecular heterogeneity of this polyp subtype. TSAs with KRAS mutation may have different malignant potential than TSAs with BRAF mutation. The recent availability of an antibody that reliably detects BRAF mutation by immunohistochemistry may help in identifying serrated polyps and move towards a more molecularly based classification of colorectal polyps [119]. Detection of BRAF mutation may be particularly helpful in distinguishing SSA with extensive cytological dysplasia from conventional adenoma as these two polyps are likely to have different malignant potential. Serrated polyposis may be more prevalent than initially thought now that gastroenterologists and pathologists have become more aware of this condition. However, prospective studies are needed to assess the risk of CRC and metachronous polyps in patients diagnosed with serrated polyps and serrated polyposis. Until then, the colonoscopy surveillance guidelines are based only on a low level of evidence.
References
Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M, et al. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988;319:525–32.
Ogino S, Fuchs CS, Giovannucci E. How many molecular subtypes? Implications of the unique tumor principle in personalized medicine. Expert Rev Mol Diagn. 2012;12:621–8.
Jass JR. Classification of colorectal cancer based on correlation of clinical, morphological and molecular features. Histopathology. 2007;50:113–30.
Ogino S, Chan AT, Fuchs CS, Giovannucci E. Molecular pathological epidemiology of colorectal neoplasia: an emerging transdisciplinary and interdisciplinary field. Gut. 2011;60:397–411.
Johannsen LG, Momsen O, Jacobsen NO. Polyps of the large intestine in Aarhus, Denmark. An autopsy study. Scand J Gastroenterol. 1989;24:799–806.
Williams AR, Balasooriya BA, Day DW. Polyps and cancer of the large bowel: a necropsy study in Liverpool. Gut. 1982;23:835–42.
Forsberg AM, Kjellstrom L, Agreus L, Nixon Andreasson A, Nyhlin H, Talley NJ, et al. Prevalence of colonic neoplasia and advanced lesions in the normal population: a prospective population-based colonoscopy study. Scand J Gastroenterol. 2012;47:184–90.
Snover DC, Jass JR, Fenoglio-Preiser C, Batts KP. Serrated polyps of the large intestine: a morphologic and molecular review of an evolving concept. Am J Clin Pathol. 2005;124:380–91.
Anderson JC, Rangasamy P, Rustagi T, Myers M, Sanders M, Vaziri H, et al. Risk factors for sessile serrated adenomas. J Clin Gastroenterol. 2011;45:694–9.
Walker RG, Landmann JK, Hewett DG, Worthley DL, Buttenshaw RL, Knight N, et al. Hyperplastic polyposis syndrome is associated with cigarette smoking, which may be a modifiable risk factor. Am J Gastroenterol. 2010;105:1642–7.
Samowitz WS, Albertsen H, Sweeney C, Herrick J, Caan BJ, Anderson KE, et al. Association of smoking, CpG island methylator phenotype, and V600E BRAF mutations in colon cancer. J Natl Cancer Inst. 2006;98:1731–8.
English DR, Young JP, Simpson JA, Jenkins MA, Southey MC, Walsh MD, et al. Ethnicity and risk for colorectal cancers showing somatic BRAF V600E mutation or CpG island methylator phenotype. Cancer Epidemiol Biomarkers Prev. 2008;17:1774–80.
Young J, Barker MA, Simms LA, Walsh MD, Biden KG, Buchanan D, et al. Evidence for BRAF mutation and variable levels of microsatellite instability in a syndrome of familial colorectal cancer. Clin Gastroenterol Hepatol. 2005;3:254–63.
Buchanan DD, Sweet K, Drini M, Jenkins MA, Win AK, English DR, et al. Risk factors for colorectal cancer in patients with multiple serrated polyps: a cross-sectional case series from genetics clinics. PLoS ONE. 2010;5:e11636.
Buchanan DD, Sweet K, Drini M, Jenkins MA, Win AK, Gattas M, et al. Phenotypic diversity in patients with multiple serrated polyps: a genetics clinic study. Int J Colorectal Dis. 2010;25:703–12.
Wish TA, Hyde AJ, Parfrey PS, Green JS, Younghusband HB, Simms MI, et al. Increased cancer predisposition in family members of colorectal cancer patients harboring the p.V600E BRAF mutation: a population-based study. Cancer Epidemiol Biomarkers Prev. 2010;19:1831–9.
Pai RK, Hart J, Noffsinger AE. Sessile serrated adenomas strongly predispose to synchronous serrated polyps in non-syndromic patients. Histopathology. 2010;56:581–8.
Pai RK, Mackinnon AC, Joseph L, Noffsinger A, Hart J. Identification of histologically distinct conventional adenomas that arise predominately in patients with sessile serrated adenomas. Am J Surg Pathol. 2010;34:355–63.
Spring KJ, Zhao ZZ, Karamatic R, Walsh MD, Whitehall VL, Pike T, et al. High prevalence of sessile serrated adenomas with BRAF mutations: a prospective study of patients undergoing colonoscopy. Gastroenterology. 2006;131:1400–7.
Carragher LA, Snell KR, Giblett SM, Aldridge VS, Patel B, Cook SJ, et al. V600EBraf induces gastrointestinal crypt senescence and promotes tumour progression through enhanced CpG methylation of p16INK4a. EMBO Mol Med. 2010;2:458–71.
Snover DC, Ahnen DJ, Burt RW, Odze RD. Serrated polyps of the colon and rectum and serrated polyposis. In: Bosman FT, Carneiro F, Hruban RH, et al, editors. WHO classification of tumours of the digestive system. Lyon, France: IARC; 2010. p. 160–5.
Snover DC. Update on the serrated pathway to colorectal carcinoma. Hum Pathol. 2011;42:1–10.
Torlakovic EE, Gomez JD, Driman DK, Parfitt JR, Wang C, Benerjee T, et al. Sessile serrated adenoma (SSA) vs. traditional serrated adenoma (TSA). Am J Surg Pathol. 2008;32:21–9.
Groff RJ, Nash R, Ahnen DJ. Significance of serrated polyps of the colon. Curr Gastroenterol Rep. 2008;10:490–8.
Kim KM, Lee EJ, Kim YH, Chang DK, Odze RD. KRAS mutations in traditional serrated adenomas from Korea herald an aggressive phenotype. Am J Surg Pathol. 2010;34:667–75.
Wong NA, Hunt LP, Novelli MR, Shepherd NA, Warren BF. Observer agreement in the diagnosis of serrated polyps of the large bowel. Histopathology. 2009;55:63–6.
Khalid O, Radaideh S, Cummings OW, O’Brien MJ, Goldblum JR, Rex DK. Reinterpretation of histology of proximal colon polyps called hyperplastic in 2001. World J Gastroenterol. 2009;15:3767–70.
Bustamante-Balen M, Bernet L, Cano R, Morell L, Lopez A. Assessing the reproducibility of the microscopic diagnosis of sessile serrated adenoma of the colon. Rev Esp Enferm Dig. 2009;101:258–64.
Farris AB, Misdraji J, Srivastava A, Muzikansky A, Deshpande V, Lauwers GY, et al. Sessile serrated adenoma: challenging discrimination from other serrated colonic polyps. Am J Surg Pathol. 2008;32:30–5.
Singh H, Bay D, Ip S, Bernstein CN, Nugent Z, Gheorghe R, et al. Pathological reassessment of hyperplastic colon polyps in a city-wide pathology practice: implications for polyp surveillance recommendations. Gastrointest Endosc. 2012;76:1003–8.
Ensari A, Bilezikci B, Carneiro F, Dogusoy GB, Driessen A, Dursun A, et al. Serrated polyps of the colon: how reproducible is their classification? Virchows Arch. 2012;461:495–504.
Rajagopalan H, Bardelli A, Lengauer C, Kinzler KW, Vogelstein B, Velculescu VE. Tumorigenesis: RAF/RAS oncogenes and mismatch-repair status. Nature. 2002;418:934.
Rosty C, Parry S, Young JP. Serrated polyposis: an enigmatic model of colorectal cancer predisposition. Patholog Res Int. 2011;2011:157073.
Rosenberg DW, Yang S, Pleau DC, Greenspan EJ, Stevens RG, Rajan TV, et al. Mutations in BRAF and KRAS differentially distinguish serrated versus non-serrated hyperplastic aberrant crypt foci in humans. Cancer Res. 2007;67:3551–4.
O’Brien MJ, Yang S, Mack C, Xu H, Huang CS, Mulcahy E, et al. Comparison of microsatellite instability, CpG island methylation phenotype, BRAF and KRAS status in serrated polyps and traditional adenomas indicates separate pathways to distinct colorectal carcinoma end points. Am J Surg Pathol. 2006;30:1491–501.
Mohammadi M, Kristensen MH, Nielsen HJ, Bonde JH, Holck S. Qualities of sessile serrated adenoma/polyp/lesion and its borderline variant in the context of synchronous colorectal carcinoma. J Clin Pathol. 2012;65:924–7.
Carr NJ, Mahajan H, Tan KL, Hawkins NJ, Ward RL. Serrated and non-serrated polyps of the colorectum: their prevalence in an unselected case series and correlation of BRAF mutation analysis with the diagnosis of sessile serrated adenoma. J Clin Pathol. 2009;62:516–8.
Kaji E, Uraoka T, Kato J, Hiraoka S, Suzuki H, Akita M, et al. Externalization of saw-tooth architecture in small serrated polyps implies the presence of methylation of IGFBP7. Dig Dis Sci. 2012;57:1261–70.
Kambara T, Simms LA, Whitehall VL, Spring KJ, Wynter CV, Walsh MD, et al. BRAF mutation is associated with DNA methylation in serrated polyps and cancers of the colorectum. Gut. 2004;53:1137–44.
Yachida S, Mudali S, Martin SA, Montgomery EA, Iacobuzio-Donahue CA. Beta-catenin nuclear labeling is a common feature of sessile serrated adenomas and correlates with early neoplastic progression after BRAF activation. Am J Surg Pathol. 2009;33:1823–32.
Fujita K, Yamamoto H, Matsumoto T, Hirahashi M, Gushima M, Kishimoto J, et al. Sessile serrated adenoma with early neoplastic progression: a clinicopathologic and molecular study. Am J Surg Pathol. 2011;35:295–304.
Fu B, Yachida S, Morgan R, Zhong Y, Montgomery EA, Iacobuzio-Donahue CA. Clinicopathologic and genetic characterization of traditional serrated adenomas of the colon. Am J Clin Pathol. 2012;138:356–66.
Han Y, Zhou ZY. Clinical features and molecular alterations of traditional serrated adenoma in sporadic colorectal carcinogenesis. J Dig Dis. 2011;12:193–8.
Kim KM, Lee EJ, Ha S, Kang SY, Jang KT, Park CK, et al. Molecular features of colorectal hyperplastic polyps and sessile serrated adenoma/polyps from Korea. Am J Surg Pathol. 2011;35:1274–86.
Worthley DL, Whitehall VL, Buttenshaw RL, Irahara N, Greco SA, Ramsnes I, et al. DNA methylation within the normal colorectal mucosa is associated with pathway-specific predisposition to cancer. Oncogene. 2010;29:1653–62.
Dhir M, Yachida S, Van Neste L, Glockner SC, Jeschke J, Pappou EP, et al. Sessile serrated adenomas and classical adenomas: an epigenetic perspective on premalignant neoplastic lesions of the gastrointestinal tract. Int J Cancer. 2011;129:1889–98.
Kriegl L, Neumann J, Vieth M, Greten FR, Reu S, Jung A, et al. Up and downregulation of p16(Ink4a) expression in BRAF-mutated polyps/adenomas indicates a senescence barrier in the serrated route to colon cancer. Mod Pathol. 2011;24:1015–22.
Fu X, Li J, Li K, Tian X, Zhang Y. Hypermethylation of APC promoter 1A is associated with moderate activation of Wnt signalling pathway in a subset of colorectal serrated adenomas. Histopathology. 2009;55:554–63.
Fu X, Yang X, Chen K, Zhang Y. Retained cell-cell adhesion in serrated neoplastic pathway as opposed to conventional colorectal adenomas. J Histochem Cytochem. 2011;59:158–66.
Jiao YF, Nakamura S, Sugai T, Yamada N, Habano W. Serrated adenoma of the colorectum undergoes a proliferation versus differentiation process: new conceptual interpretation of morphogenesis. Oncology. 2008;74:127–34.
Joo M, Shahsafaei A, Odze RD. Paneth cell differentiation in colonic epithelial neoplasms: evidence for the role of the Apc/beta-catenin/Tcf pathway. Hum Pathol. 2009;40:872–80.
Oh K, Redston M, Odze RD. Support for hMLH1 and MGMT silencing as a mechanism of tumorigenesis in the hyperplastic-adenoma-carcinoma (serrated) carcinogenic pathway in the colon. Hum Pathol. 2005;36:101–11.
Sandmeier D, Benhattar J, Martin P, Bouzourene H. Serrated polyps of the large intestine: a molecular study comparing sessile serrated adenomas and hyperplastic polyps. Histopathology. 2009;55:206–13.
Sawyer EJ, Cerar A, Hanby AM, Gorman P, Arends M, Talbot IC, et al. Molecular characteristics of serrated adenomas of the colorectum. Gut. 2002;51:200–6.
Wu JM, Montgomery EA, Iacobuzio-Donahue CA. Frequent beta-catenin nuclear labeling in sessile serrated polyps of the colorectum with neoplastic potential. Am J Clin Pathol. 2008;129:416–23.
Yamamoto T, Konishi K, Yamochi T, Makino R, Kaneko K, Shimamura T, et al. No major tumorigenic role for beta-catenin in serrated as opposed to conventional colorectal adenomas. Br J Cancer. 2003;89:152–7.
Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–7.
Guo RJ, Funakoshi S, Lee HH, Kong J, Lynch JP. The intestine-specific transcription factor Cdx2 inhibits beta-catenin/TCF transcriptional activity by disrupting the beta-catenin-TCF protein complex. Carcinogenesis. 2010;31:159–66.
Kohonen-Corish MR, Sigglekow ND, Susanto J, Chapuis PH, Bokey EL, Dent OF, et al. Promoter methylation of the mutated in colorectal cancer gene is a frequent early event in colorectal cancer. Oncogene. 2007;26:4435–41.
Wajapeyee N, Serra RW, Zhu X, Mahalingam M, Green MR. Oncogenic BRAF induces senescence and apoptosis through pathways mediated by the secreted protein IGFBP7. Cell. 2008;132:363–74.
Waye JD, Bilotta JJ. Rectal hyperplastic polyps: now you see them, now you don’t—a differential point. Am J Gastroenterol. 1990;85:1557–9.
Rondagh EJ, Masclee AA, Bouwens MW, Winkens B, Riedl RG, de Bruine AP, et al. Endoscopic red flags for the detection of high-risk serrated polyps: an observational study. Endoscopy. 2011;43:1052–8.
Tadepalli US, Feihel D, Miller KM, Itzkowitz SH, Freedman JS, Kornacki S, et al. A morphologic analysis of sessile serrated polyps observed during routine colonoscopy (with video). Gastrointest Endosc. 2011;74:1360–8.
Hasegawa S, Mitsuyama K, Kawano H, Arita K, Maeyama Y, Akagi Y, et al. Endoscopic discrimination of sessile serrated adenomas from other serrated lesions. Oncol Lett. 2011;2:785–9.
Rex DK, Hewett DG, Snover DC. Editorial: detection targets for colonoscopy: from variable detection to validation. Am J Gastroenterol. 2010;105:2665–9.
Rex DK. Update on colonoscopic imaging and projections for the future. Clin Gastroenterol Hepatol. 2010;8:318–21.
Hewett DG, Kaltenbach T, Sano Y, Tanaka S, Saunders BP, Ponchon T, et al. Validation of a simple classification system for endoscopic diagnosis of small colorectal polyps using narrow-band imaging. Gastroenterology. 2012;143:599–607.
Rex DK, Ahnen DJ, Baron JA, Batts KP, Burke CA, Burt RW, et al. Serrated lesions of the colorectum: review and recommendations from an expert panel. Am J Gastroenterol. 2012;107:1315–29.
Kimura T, Yamamoto E, Yamano HO, Suzuki H, Kamimae S, Nojima M, et al. A novel pit pattern identifies the precursor of colorectal cancer derived from sessile serrated adenoma. Am J Gastroenterol. 2012;107:460–9.
Sandmeier D, Seelentag W, Bouzourene H. Serrated polyps of the colorectum: is sessile serrated adenoma distinguishable from hyperplastic polyp in a daily practice? Virchows Arch. 2007;450:613–8.
Hewett DG, Kahi CJ, Rex DK. Does colonoscopy work? J Natl Compr Canc Netw. 2010;8:67–76.
Hewett DG, Kahi CJ, Rex DK. Efficacy and effectiveness of colonoscopy: how do we bridge the gap? Gastrointest Endosc Clin N Am. 2010;20:673–84.
Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150:1–8.
Baxter NN, Sutradhar R, Forbes SS, Paszat LF, Saskin R, Rabeneck L. Analysis of administrative data finds endoscopist quality measures associated with postcolonoscopy colorectal cancer. Gastroenterology. 2011;140:65–72.
Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011;154:22–30.
Brenner H, Hoffmeister M, Arndt V, Stegmaier C, Altenhofen L, Haug U. Protection from right- and left-sided colorectal neoplasms after colonoscopy: population-based study. J Natl Cancer Inst. 2010;102:89–95.
Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010;139:1128–37.
Singh H, Nugent Z, Demers AA, Bernstein CN. Rate and predictors of early/missed colorectal cancers after colonoscopy in Manitoba: a population-based study. Am J Gastroenterol. 2010;105:2588–96.
Burnett-Hartman AN, Newcomb PA, Phipps AI, Passarelli MN, Grady WM, Upton MP, et al. Colorectal endoscopy, advanced adenomas, and sessile serrated polyps: implications for proximal colon cancer. Am J Gastroenterol. 2012;107:1213–9.
Hiraoka S, Kato J, Fujiki S, Kaji E, Morikawa T, Murakami T, et al. The presence of large serrated polyps increases risk for colorectal cancer. Gastroenterology. 2010;139:1503–10.
Arain MA, Sawhney M, Sheikh S, Anway R, Thyagarajan B, Bond JH, et al. CIMP status of interval colon cancers: another piece to the puzzle. Am J Gastroenterol. 2010;105:1189–95.
Sawhney MS, Farrar WD, Gudiseva S, Nelson DB, Lederle FA, Rector TS, et al. Microsatellite instability in interval colon cancers. Gastroenterology. 2006;131:1700–5.
Hetzel JT, Huang CS, Coukos JA, Omstead K, Cerda SR, Yang S, et al. Variation in the detection of serrated polyps in an average risk colorectal cancer screening cohort. Am J Gastroenterol. 2010;105:2656–64.
Kahi CJ, Hewett DG, Norton DL, Eckert GJ, Rex DK. Prevalence and variable detection of proximal colon serrated polyps during screening colonoscopy. Clin Gastroenterol Hepatol. 2011;9:42–6.
Hill A, Horswill MS, Plooy AM, Watson MO, Rowlands L, Wallis GM, et al. The development and validation of a colorectal polyp recognition test. J Gastroenterol Hepatol. 2011;26:32.
Hewett DG, Rex DK. Cap-fitted colonoscopy: a randomized, tandem colonoscopy study of adenoma miss rates. Gastrointest Endosc. 2010;72:775–81.
Hewett DG, Rex DK. Miss rate of right-sided colon examination during colonoscopy defined by retroflexion: an observational study. Gastrointest Endosc. 2011;74:246–52.
Subramanian V, Mannath J, Hawkey CJ, Ragunath K. High definition colonoscopy vs. standard video endoscopy for the detection of colonic polyps: a meta-analysis. Endoscopy. 2011;43:499–505.
Dinesen L, Chua TJ, Kaffes AJ. Meta-analysis of narrow-band imaging versus conventional colonoscopy for adenoma detection. Gastrointest Endosc. 2012;75:604–11.
Kahi CJ, Anderson JC, Waxman I, Kessler WR, Imperiale TF, Li X, et al. High-definition chromocolonoscopy vs. high-definition white light colonoscopy for average-risk colorectal cancer screening. Am J Gastroenterol. 2010;105:1301–7.
Pohl J, Schneider A, Vogell H, Mayer G, Kaiser G, Ell C. Pancolonic chromoendoscopy with indigo carmine versus standard colonoscopy for detection of neoplastic lesions: a randomised two-centre trial. Gut. 2011;60:485–90.
Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson DA, Levin TR. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143:844–57.
Holt BA, Bourke MJ. Wide field endoscopic resection for advanced colonic mucosal neoplasia: current status and future directions. Clin Gastroenterol Hepatol. 2012;10:969–79.
Hewett DG, Rex DK. Colonoscopy and diminutive polyps: hot or cold biopsy or snare? Do I send to pathology? Clin Gastroenterol Hepatol. 2011;9:102–5.
Pohl E, Srivastava A, Bensen SP, Anderson P, Rothstein RI, Gordon SR, et al. Incomplete polyp resection during colonoscopy—results of the Complete Adenoma Resection (CARE) Study. Gastroenterology. 2012. doi:10.1053/j.gastro.2012.09.043.
Goldstein NS, Bhanot P, Odish E, Hunter S. Hyperplastic-like colon polyps that preceded microsatellite-unstable adenocarcinomas. Am J Clin Pathol. 2003;119:778–96.
Schreiner MA, Weiss DG, Lieberman DA. Proximal and large hyperplastic and nondysplastic serrated polyps detected by colonoscopy are associated with neoplasia. Gastroenterology. 2010;139:1497–502.
Oono Y, Fu K, Nakamura H, Iriguchi Y, Yamamura A, Tomino Y, et al. Progression of a sessile serrated adenoma to an early invasive cancer within 8 months. Dig Dis Sci. 2009;54:906–9.
Lash RH, Genta RM, Schuler CM. Sessile serrated adenomas: prevalence of dysplasia and carcinoma in 2139 patients. J Clin Pathol. 2010;63:681–6.
Lu FI, van Niekerk de W, Owen D, Tha SP, Turbin DA, Webber DL. Longitudinal outcome study of sessile serrated adenomas of the colorectum: an increased risk for subsequent right-sided colorectal carcinoma. Am J Surg Pathol. 2010;34:927–34.
Teriaky A, Driman DK, Chande N. Outcomes of a 5-year follow-up of patients with sessile serrated adenomas. Scand J Gastroenterol. 2012;47:178–83.
Salaria SN, Streppel MM, Lee LA, Iacobuzio-Donahue CA, Montgomery EA. Sessile serrated adenomas: high-risk lesions? Hum Pathol. 2012;43:1808–14.
Winawer SJ, Zauber AG, Fletcher RH, Stillman JS, O’Brien MJ, Levin B, et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. Gastroenterology. 2006;130:1872–85.
Moss A, Bourke MJ, Williams SJ, Hourigan LF, Brown G, Tam W, et al. Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology. 2011;140:1909–18.
Terdiman JP, McQuaid KR. Surveillance guidelines should be updated to recognize the importance of serrated polyps. Gastroenterology. 2010;139:1444–7.
Biswas S, Ellis AJ, Guy R, Savage H, Madronal K, East JE. High prevalence of hyperplastic polyposis syndrome (serrated polyposis) in the NHS bowel cancer screening programme. Gut. 2012. doi:10.1136/gutjnl-2012-303233.
Crowder CD, Sweet K, Lehman A, Frankel WL. Serrated polyposis is an underdiagnosed and unclear syndrome: the surgical pathologist has a role in improving detection. Am J Surg Pathol. 2012;36:1178–85.
Moreira L, Pellise M, Carballal S, Bessa X, Ocana T, Serradesanferm A, et al. High prevalence of serrated polyposis syndrome in FIT-based colorectal cancer screening programmes. Gut. 2012. doi:10.1136/gutjnl-2012-303496.
Vemulapalli KC, Rex DK. Failure to recognize serrated polyposis syndrome in a cohort with large sessile colorectal polyps. Gastrointest Endosc. 2012;75:1206–10.
Rosty C, Buchanan DD, Walsh MD, Pearson SA, Pavluk E, Walters RJ, et al. Phenotype and polyp landscape in serrated polyposis syndrome: a series of 100 patients from genetics clinics. Am J Surg Pathol. 2012;36:876–82.
Boparai KS, Mathus-Vliegen EM, Koornstra JJ, Nagengast FM, van Leerdam M, van Noesel CJ, et al. Increased colorectal cancer risk during follow-up in patients with hyperplastic polyposis syndrome: a multicentre cohort study. Gut. 2010;59:1094–100.
Boparai KS, Reitsma JB, Lemmens V, van Os TA, Mathus-Vliegen EM, Koornstra JJ, et al. Increased colorectal cancer risk in first-degree relatives of patients with hyperplastic polyposis syndrome. Gut. 2010;59:1222–5.
Win AK, Walters RJ, Buchanan DD, Jenkins MA, Sweet K, Frankel WL, et al. Cancer risks for relatives of patients with serrated polyposis. Am J Gastroenterol. 2012;107:770–8.
Young JP, Parry S. Risk factors: hyperplastic polyposis syndrome and risk of colorectal cancer. Nat Rev Gastroenterol Hepatol. 2010;7:594–5.
Gurudu SR, Heigh RI, De Petris G, Heigh EG, Leighton JA, Pasha SF, et al. Sessile serrated adenomas: demographic, endoscopic and pathological characteristics. World J Gastroenterol. 2010;16:3402–5.
Torlakovic E, Skovlund E, Snover DC, Torlakovic G, Nesland JM. Morphologic reappraisal of serrated colorectal polyps. Am J Surg Pathol. 2003;27:65–81.
Goldstein NS. Small colonic microsatellite unstable adenocarcinomas and high-grade epithelial dysplasias in sessile serrated adenoma polypectomy specimens: a study of eight cases. Am J Clin Pathol. 2006;125:132–45.
Sheridan TB, Fenton H, Lewin MR, Burkart AL, Iacobuzio-Donahue CA, Frankel WL, et al. Sessile serrated adenomas with low- and high-grade dysplasia and early carcinomas: an immunohistochemical study of serrated lesions “caught in the act”. Am J Clin Pathol. 2006;126:564–71.
Capper D, Preusser M, Habel A, Sahm F, Ackermann U, Schindler G et al. Assessment of BRAF V600E mutation status by immunohistochemistry with a mutation-specific monoclonal antibody. Acta Neuropathol. 2011;122:11–9.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 2.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc/2.0/.
About this article
Cite this article
Rosty, C., Hewett, D.G., Brown, I.S. et al. Serrated polyps of the large intestine: current understanding of diagnosis, pathogenesis, and clinical management. J Gastroenterol 48, 287–302 (2013). https://doi.org/10.1007/s00535-012-0720-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-012-0720-y