Key Points
-
Malaria, caused by Plasmodium spp., remains a tremendous disease burden worldwide, causing nearly one million deaths and 250 million cases of disease.
-
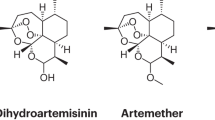
Artemisinin and artemisinin derivatives are effective antimalarials, especially when coupled with a second, unrelated antimalarial.
-
Owing to the use of artemisinin as a monotherapy, strains of Plasmodium falciparum have emerged that have a decreased sensitivity to the drug.
-
Several strategies to prevent the spread of the less resistant parasites have been put in place, such as a multifaceted approach that includes early diagnosis and appropriate treatment, decreasing drug pressure, optimising vector control, targeting the mobile population, strengthening of management and surveillance systems, and operations research.
-
Other, broader strategies can target the emergence and spread of drug resistance. These include mass drug administration, using multiple first-line therapies simultaneously, surveillance, active case investigation and focal control
Abstract
Artemisinin combination therapies are the first-line treatments for uncomplicated Plasmodium falciparum malaria in most malaria-endemic countries. Recently, partial artemisinin-resistant P. falciparum malaria has emerged on the Cambodia–Thailand border. Exposure of the parasite population to artemisinin monotherapies in subtherapeutic doses for over 30 years, and the availability of substandard artemisinins, have probably been the main driving force in the selection of the resistant phenotype in the region. A multifaceted containment programme has recently been launched, including early diagnosis and appropriate treatment, decreasing drug pressure, optimising vector control, targeting the mobile population, strengthening management and surveillance systems, and operational research. Mathematical modelling can be a useful tool to evaluate possible strategies for containment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
World Health Organisation. WHO guidelines for the treatment of malaria. (WHO, Geneva, 2006).
Baird, J. K. Effectiveness of antimalarial drugs. N. Engl. J. Med. 352, 1565–1577 (2005).
Korenromp, E. L., Williams, B. G., Gouws, E., Dye, C. & Snow, R. W. Measurement of trends in childhood malaria mortality in Africa: an assessment of progress toward targets based on verbal autopsy. Lancet Infect. Dis. 3, 349–358 (2003). One of the few studies directly linking antimalarial drug resistance to an increase in mortality of African children that is due to malaria.
Trape, J. F. et al. Impact of chloroquine resistance on malaria mortality. C. R. Acad. Sci. III 321, 689–697 (1998).
Barnes, K. I. et al. Effect of artemether-lumefantrine policy and improved vector control on malaria burden in KwaZulu-Natal, South Africa. PLoS Med. 2, e330 (2005). The first of several studies from a wide range of geographical areas showing the contribution ACTs to a reduction in malaria burden,
Bhattarai, A. et al. Impact of artemisinin-based combination therapy and insecticide-treated nets on malaria burden in Zanzibar. PLoS Med. 4, e309 (2007).
Carrara, V. I. et al. Deployment of early diagnosis and mefloquine-artesunate treatment of falciparum malaria in Thailand: the Tak Malaria Initiative. PLoS Med. 3, e183 (2006).
O'Meara, W. P. et al. Effect of a fall in malaria transmission on morbidity and mortality in Kilifi, Kenya. Lancet 372, 1555–1562 (2008).
Dondorp, A., Nosten, F., Stepniewska, K., Day, N. & White, N. Artesunate versus quinine for treatment of severe falciparum malaria: a randomised trial. Lancet 366, 717–725 (2005). Large trial from Southeast Asia showing a 35% reduction in mortality in patients with severe malaria that were treated with artesunate compared with those treated with quinine.
Meshnick, S. R., Taylor, T. E. & Kamchonwongpaisan, S. Artemisinin and the antimalarial endoperoxides: from herbal remedy to targeted chemotherapy. Microbiol. Rev. 60, 301–315 (1996).
White, N. J. Qinghaosu (artemisinin): the price of success. Science 320, 330–334 (2008). Excellent overview on the artemisinin derivatives as the most potent antimalarial drugs to date.
Adjuik, M. et al. Artesunate combinations for treatment of malaria: meta-analysis. Lancet 363, 9–17 (2004). Meta-analysis showing the superiority of ACTs for the treatment of uncomplicated P. falciparum malaria.
Okell, L. C., Drakeley, C. J., Ghani, A. C., Bousema, T. & Sutherland, C. J. Reduction of transmission from malaria patients by artemisinin combination therapies: a pooled analysis of six randomized trials. Malar. J. 7, 125 (2008).
Pukrittayakamee, S. et al. Activities of artesunate and primaquine against asexual- and sexual-stage parasites in falciparum malaria. Antimicrob. Agents Chemother. 48, 1329–1334 (2004).
Stepniewska, K. & White, N. J. Pharmacokinetic determinants of the window of selection for antimalarial drug resistance. Antimicrob. Agents Chemother. 52, 1589–1596 (2008).
White, N. J. & Olliaro, P. L. Strategies for the prevention of antimalarial drug resistance: rationale for combination chemotherapy for malaria. Parasitol. Today 12, 399–401 (1996).
White, N. J. Antimalarial drug resistance. J. Clin.Invest. 113, 1084–1092 (2004). Review on the theoretical background and mechanisms underlying emergence and spread of antimalarial drug resistance.
White, N. J. et al. Hyperparasitaemia and low dosing are an important source of anti-malarial drug resistance. Malar. J. 8, 253 (2009).
World Health Organisation. World Malaria Report 2008. (WHO, Geneva, 2008).
Olliaro, P. & Wells, T. N. The global portfolio of new antimalarial medicines under development. Clin. Pharmacol. Ther. 85, 2584–595 (2009). Overview of the current portfolio of new antimalarial drugs, almost exclusively relying on ACTs.
Resistance to artemisinin derivatives along the Thai-Cambodian border. Wkly Epidemiol. Rec. 82, 360 (2007).
Denis, M. B. et al. Surveillance of the efficacy of artesunate and mefloquine combination for the treatment of uncomplicated falciparum malaria in Cambodia. Trop. Med. Int. Health 11, 1360–1366 (2006).
Alker, A. P. et al. Pfmdr1 and in vivo resistance to artesunate-mefloquine in falciparum malaria on the Cambodian-Thai border. Am. J. Trop. Med. Hyg. 76, 641–647 (2007).
Wongsrichanalai, C. & Meshnick, S. R. Declining artesunate-mefloquine efficacy against falciparum malaria on the Cambodia-Thailand border. Emerg. Infect. Dis. 14, 716–719 (2008).
Noedl, H., Socheat, D. & Satimai, W. Artemisinin-resistant malaria in Asia. N. Engl. J. Med. 361, 540–541 (2009). One of the first detailed reports on emerging artemisinin resistance in western Cambodia.
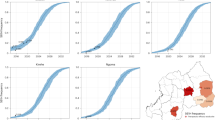
Dondorp, A. M. et al. Artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 361, 455–467 (2009). Hallmark study showing a clear reduction in in vivo P. falciparum susceptibility to artesunate on the Cambodia–Thailand border.
Anderson, T. et al. High heritability of malaria parasite clearance rates indicates a genetic basis for artemisinin resistance in Western Cambodia. J. Infect. Dis. (in the press).
Yeung, S., Van Damme, W., Socheat, D., White, N. J. & Mills, A. Access to artemisinin combination therapy for malaria in remote areas of Cambodia. Malar. J. 7, 96 (2008). Study showing that treatment of uncomplicated P. falciparum malaria in remote areas of Cambodia is mainly through the less well-controlled private sector, in which artemisinin monotherapies are widely available.
Newton, P. N., Dondorp, A., Green, M., Mayxay, M. & White, N. J. Counterfeit artesunate antimalarials in southeast Asia. Lancet 362, 169 (2003). Article highlighting the terrible problem of the wide availability of counterfeited artemisinins in Southeast Asia.
Rathod, P. K., McErlean, T. & Lee, P. C. Variations in frequencies of drug resistance in Plasmodium falciparum. Proc. Natl Acad. Sci. USA 94, 9389–9393 (1997).
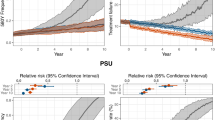
Pongtavornpinyo, W. et al. Spread of anti-malarial drug resistance: mathematical model with implications for ACT drug policies. Malar. J. 7, 229 (2008). Modelling paper investigating the minimal public health conditions, such as ACT coverage rates, that are necessary to delay the spread of antimalarial drug resistance.
Maude, R. J. et al. The role of mathematical modelling in malaria elimination and eradication. Trans. R. Soc. Trop. Med. Hyg. 103, 643–644 (2009).
Verdrager, J. Epidemiology of the emergence and spread of drug-resistant falciparum malaria in South-East Asia and Australasia. J. Trop. Med. Hyg. 89, 277–289 (1986).
Verdrager, J. Localized permanent epidemics: the genesis of chloroquine resistance in Plasmodium falciparum. Southeast Asian J. Trop.Med. Public Health 26, 23–28 (1995).
Carrara, V. I. et al. Changes in the treatment responses to artesunate-mefloquine on the northwestern border of Thailand during 13 years of continuous deployment. PLoS ONE 4, e4551 (2009). First study reporting a slight decrease in treatment responses to an ACT for uncomplicated P. falciparum malaria in an area outside the Cambodia–Thailand border region.
Achan, J. et al. Effectiveness of quinine versus artemether-lumefantrine for treating uncomplicated falciparum malaria in Ugandan children: randomised trial. BMJ 339, b2763 (2009).
Gebru, T., Hailu, A., Kremsner, P. G., Kun, J. F. & Grobusch, M. P. Molecular surveillance of mutations in the cytochrome b gene of Plasmodium falciparum in Gabon and Ethiopia. Malar. J. 5, 112 (2006).
Olliaro, P. & Mussano, P. Amodiaquine for treating malaria. Cochrane Database Syst. Rev. 2003, CD000016 (2003).
Gesase, S. et al. High resistance of Plasmodium falciparum to sulphadoxine/pyrimethamine in northern Tanzania and the emergence of dhps resistance mutation at codon 581. PLoS ONE 4, e4569 (2009).
Pilz, J. B. et al. In vitro sensitivity of Plasmodium falciparum to lumefantrine in north-western Thailand. Wien. Klin. Wochenschr. 116 (Suppl. 4), 41–46 (2004).
Wongsrichanalai, C., Pickard, A. L., Wernsdorfer, W. H. & Meshnick, S. R. Epidemiology of drug-resistant malaria. Lancet Infect. Dis. 2, 209–218 (2002).
von Seidlein, L. & Greenwood, B. M. Mass administrations of antimalarial drugs. Trends Parasitol. 19, 452–460 (2003).
Tran, T. H. et al. Dihydroartemisinin-piperaquine against multidrug-resistant Plasmodium falciparum malaria in Vietnam: randomised clinical trial. Lancet 363, 18–22 (2004).
Ramharter, M. et al. Fixed-dose pyronaridine-artesunate combination for treatment of uncomplicated falciparum malaria in pediatric patients in Gabon. J. Infect. Dis. 198, 911–919 (2008).
Vivas, L. et al. Anti-malarial efficacy of pyronaridine and artesunate in combination in vitro and in vivo. Acta Trop. 105, 222–228 (2008).
Ringwald, P., Bickii, J. & Basco, L. Randomised trial of pyronaridine versus chloroquine for acute uncomplicated falciparum malaria in Africa. Lancet 347, 24–28 (1996).
Carr, A. & Amin, J. Efficacy and tolerability of initial antiretroviral therapy: a systematic review. AIDS 23, 343–353 (2009).
Grant, A., Gothard, P. & Thwaites, G. Managing drug resistant tuberculosis. BMJ 337, a1110 (2008).
Lawpoolsri, S. et al. Optimally timing primaquine treatment to reduce Plasmodium falciparum transmission in low endemicity Thai-Myanmar border populations. Malar. J. 8, 159 (2009).
Vale, N., Moreira, R. & Gomes, P. Primaquine revisited six decades after its discovery. Eur. J. Med. Chem. 44, 937–953 (2009).
Cappellini, M. D. & Fiorelli, G. Glucose-6-phosphate dehydrogenase deficiency. Lancet 371, 64–74 (2008).
[No authors listed]. Roll Back Malaria Partnership. Global Malaria Action Plan for a malaria-free world[online] (2009).
Samarasekera, U. Countries race to contain resistance to key antimalarial. Lancet 374, 277–280 (2009).
Maude, R. J. et al. The last man standing is the most resistant: eliminating artemisinin-resistant malaria in Cambodia. Malar. J. 8, 31 (2009). Modelling paper showing that the absolute number of artemisinin-resistant malaria cases will decrease, but the proportion of artemisinin-resistant malaria cases will increase over time when elimination of resistant malaria is attempted.
Korsinczky, M. et al. Mutations in Plasmodium falciparum cytochrome b that are associated with atovaquone resistance are located at a putative drug-binding site. Antimicrob. Agents Chemother. 44, 2100–2108 (2000).
Okell, L. C., Drakeley, C. J., Bousema, T., Whitty, C. J. & Ghani, A. C. Modelling the impact of artemisinin combination therapy and long-acting treatments on malaria transmission intensity. PLoS Med. 5, e226 (2008).
Castle, S. J., Toscano, N. C., Prabhaker, N., Henneberry, T. J. & Palumbo, J. C. Field evaluation of different insecticide use strategies as resistance management and control tactics for Bemisia tabaci (Hemiptera: Aleyrodidae). Bull. Entomol. Res. 92, 449–460 (2002).
Boni, M. F., Smith, D. L. & Laxminarayan, R. Benefits of using multiple first-line therapies against malaria. Proc. Natl Acad. Sci. USA 105, 14216–14221 (2008). Modelling paper showing the delay in development of antimalarial drug resistance with regional deployment of MFTs.
Shretta, R., Omumbo, J., Rapuoda, B. & Snow, R. W. Using evidence to change antimalarial drug policy in Kenya. Trop. Med. Int. Health 5, 755–764 (2000).
Coatney, G. R. Pitfalls in a discovery: the chronicle of chloroquine. Am. J. Trop. Med. Hyg. 12, 121–128 (1963).
Jensen, M. & Mehlhorn, H. Seventy-five years of Resochin in the fight against malaria. Parasitol. Res. 105, 609–627 (2009).
Greenwood, B. M. et al. Malaria: progress, perils, and prospects for eradication. J. Clin. Invest. 118, 1266–1276 (2008).
Payne, D. Spread of chloroquine resistance in Plasmodium falciparum. Parasitol.Today 3, 241–246 (1987).
Djimde, A. et al. A molecular marker for chloroquine-resistant falciparum malaria. N. Engl. J. Med. 344, 257–263 (2001).
Fidock, D. A. et al. Mutations in the P. falciparum digestive vacuole transmembrane protein PfCRT and evidence for their role in chloroquine resistance. Mol. Cell 6, 861–871 (2000).
Wootton, J. C. et al. Genetic diversity and chloroquine selective sweeps in Plasmodium falciparum. Nature 418, 320–323 (2002).
Kublin, J. G. et al. Reemergence of chloroquine-sensitive Plasmodium falciparum malaria after cessation of chloroquine use in Malawi. J. Infect. Dis. 187, 1870–1875 (2003).
Laufer, M. K. et al. Return of chloroquine antimalarial efficacy in Malawi. N. Engl. J. Med. 355, 1959–1966 (2006).
Plowe, C. V. The evolution of drug-resistant malaria. Trans. R. Soc. Trop. Med. Hyg. 103, S11–S14 (2009).
Acknowledgements
We thank N. J. White for his critical review of the paper. This work was supported by the Wellcome Trust.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Related links
DATABASES
Entrez Genome Project
FURTHER INFORMATION
Glossary
- Parenteral
-
Administered by injection.
- Recrudescence
-
Reoccurence of a disease after treatment. This can be caused by parasites that were not completely eliminated during the treatment.
- Hypnozoite
-
A dormant form of the liver stage parasites found in several Plasmodium spp., including the human parasites Plasmodium vivax and Plasmodium ovale.
Rights and permissions
About this article
Cite this article
Dondorp, A., Yeung, S., White, L. et al. Artemisinin resistance: current status and scenarios for containment. Nat Rev Microbiol 8, 272–280 (2010). https://doi.org/10.1038/nrmicro2331
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrmicro2331
This article is cited by
-
1,3-Diphenylureido hydroxamate as a promising scaffold for generation of potent antimalarial histone deacetylase inhibitors
Scientific Reports (2023)
-
Systematic review on the application of machine learning to quantitative structure–activity relationship modeling against Plasmodium falciparum
Molecular Diversity (2022)
-
Naturally acquired antibody response to a Plasmodium falciparum chimeric vaccine candidate GMZ2.6c and its components (MSP-3, GLURP, and Pfs48/45) in individuals living in Brazilian malaria-endemic areas
Malaria Journal (2022)
-
Surveillance of Plasmodium falciparum pfcrt haplotypes in southwestern Uganda by high‐resolution melt analysis
Malaria Journal (2021)
-
Addressing key gaps in implementation of mosquito larviciding to accelerate malaria vector control in southern Tanzania: results of a stakeholder engagement process in local district councils
Malaria Journal (2021)