Abstract
Prothrombin complex concentrate (PCC) is used for reversal of vitamin K antagonists (VKA) in patients with bleeding complications. This study aims to assess benefits and harms of 4-factor PCC compared to fresh frozen plasma (FFP) or no treatment in VKA associated bleeding. PubMed, EMBASE and CENTRAL were searched from 1945 to August 2015. Studies reporting 4-factor PCC use for VKA associated bleeding and providing data on INR normalization, mortality or thromboembolic (TE) complications were eligible. Two authors screened titles and full articles for inclusion, extracted data, and assessed risk of bias. Mortality data were pooled using Mantel–Haenszel random effects meta-analysis. Nineteen studies were included (N = 2878); 18 cohort studies and one RCT. Six studies had good methodological quality, 9 moderate and 4 poor. Baseline INR values ranged from 2.2 to >20. The INR within 1 h after PCC administration ranged from 1.4 to 1.9, and after FFP administration from 2.2 to 12. PCC reduced the time to reach INR correction in comparison with FFP or no treatment. The observed mortality rate ranged from 0 to 43% (mean 17%) in the PCC, 4.8–54% (mean 16%) in the FFP and 23–69% (mean 51%) in the no treatment group. Meta-analysis of mortality data resulted in an OR of 0.64 (95% confidence interval [CI] 0.27–1.5) for PCC versus FFP and an OR 0.41 (95% CI 0.13–1.3) for PCC versus no treatment. TE complications were observed in 0–18% (mean 2.5%) of PCC and in 6.4% of FFP recipients. Four-factor PCC is an effective and safe option in reversal of VKA bleeding events.
Similar content being viewed by others
Introduction
Vitamin K antagonists (VKA) are widely prescribed anticoagulant agents. Numerous trials have shown that these agents are effective in the prevention and treatment of acute and chronic venous and arterial thromboembolic diseases [1]. VKA therapy is challenging because of a narrow therapeutic window and the need for regular laboratory monitoring and dose adjustments [2, 3]. In addition, bleeding complications are a frequently observed side effect [3, 4]. Major bleeding episodes typically involve the gastrointestinal tract, urinary tract or intracranial sites and occur in 1–3% of VKA treated patients per year [5, 6]. Lethal hemorrhagic complications have an incidence of around 1% per year [5, 7]. The risk of major bleeding is associated with elevated international normalized ratios (INR); at an INR of 2.0 the bleeding risk is already increased and rises exponentially when the INR exceeds 5.0 [5, 7]. Therefore, it is no surprise that VKA top the list of medications that lead to hospital admissions [8].
Reversal of the anticoagulant effect of VKA may be required in patients with severe bleeding or in those who need to undergo an emergency invasive procedure. Depending on the clinical situation this reversal need to be completed within several hours or immediate [9]. The most straightforward intervention to counteract the effect of VKA is the administration of vitamin K [1, 10, 11]. When vitamin K is given intravenously, the INR will start to drop within 4 h of administration and will be normalized after 12–16 h [12]. Normalization of INR after oral administration of vitamin K will take up to 24 h [13].
Immediate reversal may be achieved by replacing deficient clotting factors [1, 2, 14]. In North America, fresh frozen plasma (FFP) used to be the most commonly used coagulation factor replacement product for reversal of VKA and contains factors II, VII, IX and X in a low concentration [15, 16]. Limitations of FFP use are risk of volume overload and transfusion reactions. Also, FFP is rarely able to normalize the INR completely [15,16,17,18]. Three-factor prothrombin complex concentrate (PCC) contains the vitamin K dependent coagulation factors (factors II, IX and X), as well as anticoagulant proteins C and S (and sometimes a small concentration of heparin). In addition, in 4-factor PCC preparations also coagulation factor VII is present [15, 19]. PCC provides a rapid and effective option for normalization of INR [20]. Other advantages are a reduced infusion volume and low risk of pathogen transmission [21]. In Europe, 4F-PCC has been available for decades for urgent reversal of VKA therapy. However, 4F-PCC was not approved until 2008 in Canada and 2013 in the USA, mainly due to the uncertainty of prothrombotic complications. Several international guidelines now recommend the use of PCC in reversal of VKA associated bleeding [1, 11, 22].
Several prospective studies and a few systematic reviews have been published regarding the effectiveness and safety of PCC in VKA reversal, mainly including bleeding but also non-bleeding patients requiring emergent invasive procedures, combining data on 3-factor and 4-factor PCC and predominantly addressing INR normalization or thromboembolic complications [6, 23,24,25,26]. The aim of this focused systematic review and meta-analysis was to evaluate the benefits and harms of 4-factor PCC, including INR correction, mortality, thromboembolic complications, functional outcomes and duration of hospitalization in patients with VKA associated bleeding complications. In addition, we assessed 4-factor PCC in comparison to FFP and no treatment.
Materials and methods
This systematic review and meta-analysis was performed according to the PRISMA Statement [27]. A short study protocol was composed (in Dutch) but not published online.
Search strategy
To identify all available articles on the use of 4-factor PCC in VKA related bleeding, we conducted a literature search in PubMed (1945–August 2015), EMBASE (1947–August 2015) and Cochrane Central Register of Controlled Trials (CENTRAL; 1976–August 2015) electronic databases. For PubMed and EMBASE a language filter was applied and a database specific strategy was adopted to exclude as many as possible animal studies. Details of the full search strategy can be found in Appendix I in the Supplement. Additionally, we manually searched references from four recent review articles [6, 23, 26, 28] which evaluated PCC for emergency reversal of VKA, but this revealed no new articles.
Study selection
The selection process was divided into three successive stages: title-, abstract- and full manuscript selection. Two authors (MB, KG) independently assessed the eligibility of retrieved studies according to predetermined criteria. Difference in judgment was solved by discussion.
Inclusion was based on the following criteria: the use of 4-factor PCC in patients presenting with VKA associated bleeding; and reporting on any of the following: INR normalization, number of thromboembolic events within 30 days, mortality, functional outcomes or length of stay in ICU. We included all studies using 4-factor PCC, regardless of whether or not a comparator was present. Exclusion criteria were: animal experiments; in vitro and ex vivo studies; studies that included less than 5 patients; the use of 3-factor PCC or activated 4-factor PCC; studies involving the concomitant use of recombinant factor VIIa; and studies that were duplicate reports or preliminary reports of data later presented in full (including congress abstracts).
Data extraction
Data of selected studies were extracted independently by two reviewers (MB, KG) on a structured data extraction form. Information was collected on: study design, number of patients, mean age of patients, type of bleeding, indication for PCC, type of PCC given, applied intervention, PCC dose, baseline INR, INR after intervention, ICU admission days, functional outcomes, follow-up days, mortality and thromboembolic (TE) complications.
Study quality assessment
The methodological quality of the included studies was assessed independently by two authors (MB, KG) using the Cochrane Collaboration’s tool for assessing risk of bias [29] and the Newcastle-Ottawa scale assessment of cohort and case control studies [30]. Studies were checked for selection bias, information bias, and the general validity and quality of the studies. Disagreements were solved by discussion. We qualified a study as poor, moderate or good, depending on their scores on the appropriate checklist. Since the cut-off score for each category was not defined in the literature and was up to the discretion of the author, we decided to use the following classifications in consultation with a clinical librarian (JD) and a clinical epidemiologist (BH). The maximum score on the Newcastle-Ottawa scale is 9 points. Poor outcome was assigned when the study had less than 6 points. Moderate outcome was assigned to studies with 6 points whereas more than 6 points qualified for good. The maximum score on the Cochrane Collaboration’s tool for assessing risk of bias is 7 points. Poor outcome was assigned when the study had less than 4 points, moderate was assigned to studies with 4 points and more than 4 points qualified as good.
Statistical analysis
Data are reported as mean (standard deviation [SD]), median (range), counts or percentages. Comparisons between the different treatment regimens (PCC, FFP and no treatment) were made using the Chi-square test for categorical variables (mortality, TE complications). A p-value of less than 0.05 was considered to be statistically significant. We performed an exploratory meta-analysis of the mortality data using Review Manager 5.3. The forest plots were visually examined and we assessed the statistical heterogeneity across the studies using the Cochran’s Q test and I2 values. We considered values of 25–50%, 50–75% and ≥75% to indicate low, moderate and high heterogeneity, respectively. In case of low heterogeneity, the odds ratios (OR) were combined across studies using the Mantel–Haenszel procedure which assumes a fixed treatment effect. When heterogeneity was moderate, study data were combined using a random effects model according to the method of Mantel–Haenszel.
Results
Search results
The systematic search identified 3962 articles (Medline (n = 2530); Embase (n = 1358); and CENTRAL (n = 74); see Fig. 1). Title and abstract screening identified 49 studies that were evaluated in more detail. After full article screening, we included 19 studies with a total of 2878 participants [31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49].
Characteristics of included studies
Characteristics of the included studies are shown in Table 1. Of these, 13 were prospective cohort and 5 retrospective cohort studies and one was a randomized controlled trial (RCT). The studies ranged in size from 10 to 822 patients and mean age ranged from 67 to 78 years. The most commonly observed bleeding complication was intracranial hemorrhage (ICH; 15 studies).
Many different 4-factor PCCs were used: Kanokad, Octaplex, Proplex T, Beriplex (in the USA used as Kcentra; hereafter referred to a Beriplex), PPSB-HT Nichiyaku, Kaskadil, Prothromplex and Cofact. Octaplex was the most often administered PCC. Four of the 4-factor PCC preparations contain a small amount of heparin (Beriplex, Octaplex, Kaskadil). Dosing of PCC was variable and included ‘fixed’ dose (n = 3), INR-based dosing (n = 2), weight-based dosing (n = 2) or a combination (n = 12). Six studies had good methodological quality, 9 were qualified as moderate, and 4 studies as poor.
INR normalization
Of the 19 included studies, 16 reported on INR normalization (Table 2). The administered dose of PCC ranged from 5.3 to 80 IU/kg with a typical weight-based dose of 25–50 IU/kg.
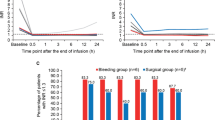
Median baseline INR values ranged from 2.2 to higher than 20. In two studies the INR measurement was repeated within 15 min of PCC administration and the median INRs were 1.1 and 1.8 respectively. Thirty minutes after PCC administration, the INR ranged from 1.1 to 1.8 (n = 4) and after 1 h the range was 1.4–1.9 (n = 4). Time to INR <1.5 (<1.6 in one study) in the PCC groups ranged from 65 to 331 min. An hour after FFP administration the median INR was 4.5 (range 2.2–12.2) in one study. The INR normalized to <1.5 on average in 256 min in the FFP group (n = 1) and in 738 min in the no treatment group (n = 1).
Three studies compared INR normalization between PCC and FFP regimens. A prospective cohort study showed that the time to INR <1.6 was 65 min in patients treated with PCC versus 256 min in FFP treated patients [47]. Results of the RCT showed a significant reduction in time to INR normalization when PCC was used as compared to FFP (p < 0.0001) [44]. This was also observed in a prospective cohort study; after 1 h INR was normalized to 1.5 after PCC and to 4.5 after FFP administration [37]. In summary, PCC was able to reach INR correction more rapidly compared to FFP or no treatment.
Mortality
Seventeen studies assessed mortality outcomes (Table 3). The time of follow-up ranged from 7 to 90 days in 10 studies, while the duration of follow-up for the remaining studies was not clearly reported.
Overall 550 (19%) deaths were reported in 2828 patients. The mortality rate in the PCC group ranged from 0 to 43% [mean 17% (407/2436)], between 5 and 54% in FFP recipients [mean 16% (25/159)] and from 23 to 69% in the no treatment group [mean 51% (118/233)]. The mean mortality rates of patients treated with PCC and FFP were not statistically different (p = 0.73), whereas the mortality rate in the no treatment group was significantly higher than in the PCC group (p < 0.001).
Thromboembolic complications
Nine studies reported on TE complications (Table 3). A total of 61 (2.7%) TE complications were observed in 2262 patients. The range of observed TE complication rate in the PCC group was 0–18% [mean 2.5% (54/2158)]. Only one study reported on TE complications in the FFP group with a mean of 6.4% (7/104). The mean TE complication rate did not differ between patients treated with PCC or FFP (p = 0.54). No data were available on TE complications in the no treatment group.
Functional outcomes
Six studies evaluated functional outcomes (Table 3). Results of the included RCT showed similar functional outcomes between PCC and FFP on hemostatic efficacy, which is the rate of cessation of the bleeding assessed over a 24-h period after start of PCC [44]. Two studies without a control group assessed functional outcomes on the modified rankin scale (mRS) measuring the degree of disability or impairment of activities of daily life attributable to a ICH. In the first study a median mRS of 5 (severe disability) was observed in patients receiving PCC [33], and in the second 64% of PCC recipients had a mRS score of 5 or 6 [48]. Another study showed a mRS ≥ 3 (moderate to severe disability) in 10 (45%) of patients in the PCC group and in 20 (71%) of the patients in the no treatment group [38]. The other two studies did not used validated scores on functional outcomes, but showed good response to treatment [40] and excellent clinical outcomes [46].
Exploratory meta-analysis
The longest follow-up data from each of the included studies which incorporated mortality rates were used for the exploratory meta-analysis. Three studies [37, 42, 44] evaluated mortality in PCC versus FFP. The combined OR was 0.64 (95% CI 0.27–1.5; I2 = 26%; Fig. 2).
Three other studies [35, 36, 38] compared PCC versus no treatment on overall mortality. Analysis of the pooled data showed an OR of 0.41 (95% CI 0.13–1.3; I2 = 69%; Fig. 3).
Discussion
The results from the present analysis show that 4-factor PCC is a rapid and effective method to normalize INR in patients with VKA associated bleeding. PCC was shown to be more effective than FFP or no treatment in the correction of the INR to a level of 1.5 or lower. Our review also showed that mortality in patients treated with PCC was substantial, ranging from 0 to 43%, and was comparable to that in patients receiving FFP. Mortality rates were lower in the PCC group compared to no treatment. PCC therapy was associated with a low risk of TE complications, also in comparison to treatment with FFP, although based on small patient numbers from a single study. Finally, functional outcomes in PCC treated patients with VKA associated bleeding events were only assessed in a few studies and outcomes were highly variable.
To our knowledge this review is the first to describe a relatively homogeneous group of studies that all evaluated 4-factor PCC in patients with VKA associated bleeding complications (reversal for emergent interventions were not included). Moreover we included a substantial number of prospective studies and one RCT, with most of the studies of moderate or good methodological quality. Other strengths of the current project include the enhanced search strategy, the data collection and extraction by two independent researchers.
Similar findings regarding the efficacy of PCC in INR normalization have been observed in earlier reviews [6, 25, 26]. A recent Cochrane Review evaluated 4-factor PCC compared to administration of FFP in patients with VKA associated bleeding or indication for emergent procedures. The authors conclude that PCC is able to reverse VKA associated INR prolongation without further requiring FFP or other blood products [28].
The reported TE event rates from the current analysis are comparable to those from an earlier review in patients treated with 4-factor PCC [23] and another recent retrospective study evaluating the effects of 4-factor PCC [50]. In all analyses, including the present one, it is unclear in how many of the cases the PCC administration was directly related to TE events or is due to cessation of the anticoagulant treatment.
The observed mortality rate in the PCC group ranged from 0 to 43% with a mean of 17%. This rate is somewhat higher than reported in the literature in patients needing reversal with PCC for bleeding as well as surgery (11%) [23]. The high mortality rate in this review likely reflects the presence of severe intracranial bleeding in a large population of the included VKA users.
Some methodological aspects require comment. First, a limitation of our systematic review is that only one RCT could be included, while all other studies were cohort studies. As a result, causal relationships between 4-factior PCC and study outcomes cannot be made. Additionally, the results should be with interpreted with caution because in observational studies it is more likely that patients with a very poor predicted outcome at presentation receive less aggressive treatment, and therefore the patients that are selected to receive PCC have a better prognosis beforehand. Furthermore, also due to the observational nature of our data, the observed associations could possibly be explained by confounding or bias, and could therefore have overestimated or underestimated true treatment effects. To gain insight on the risk of bias in included studies, we assessed the methodological quality of these by means of validated tools. We found that in the vast majority of the studies the quality was moderate or high. Therefore we expect that the impact of bias on our study results will be limited. Secondly, in more than half of the studies there was no control group. Due to a limited number of patients in the control groups it is difficult to give a clear overview of the outcomes in efficacy between the PCC and the FFP/no treatment groups. Another aspect is the large variation in design, in- and exclusion criteria, treatment, definitions and representation of results. For example, differences in patient characteristics, PCC doses, INR standardization among laboratories, and baseline INR values between groups may have affected the response to PCC. Furthermore, the INR data provided by the included studies had different INR targets (INR <1.3–1.6) and reported on the INR outcomes in many different ways (Table 2). The large variability could have influenced the results. We tried to minimize this effect by executing a strict methodology by two researchers including a rigorous selection procedure. In addition, the results of the meta-analysis need to be interpreted with caution because they are based on an indirect comparison of studies that differed in sample size, inclusion criteria and methodological quality. Finally, vitamin K administration was not universally used in all studies, which should be kept in mind when interpreting the study outcomes.
Can these findings be translated into clinical practice? The patients included are real world patients experiencing major bleeding complications of VKA treatment. The results are therefore likely to be generalizable to other patients with VKA associated hemorrhages. However, a lot of other factors play a role, including the availability of 4-factor PCC, the resources of the hospital, the experience with VKA associated bleeding events etcetera. Current guidelines recommended the administration of PCC over FFP in patients with major bleeding, in addition to use of intravenous vitamin K [11] and our results subscribe this.
In conclusion, this study assessed clinical outcomes and laboratory measures of INR in patients with VKA-associated major bleeding events treated with 4-factor PCC. The most frequently observed bleeding was ICH. Our results indicate that 4-factor PCC is an effective and safe option for treatment of VKA associated bleeding complications. In addition, 4-factor PCC seemed to be more effective than FFP or no treatment in INR normalization without increasing the risk of TE complications and mortality.
References
Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, Svensson PJ, Veenstra DL, Crowther M, Guyatt GH (2012) Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th edn: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141:e152S–e184S. doi:10.1378/chest.11-2295
Hanley JP (2004) Warfarin reversal. J Clin Pathol 57:1132–1139. doi:10.1136/jcp.2003.008904
Baglin T (1998) Management of warfarin (coumarin) overdose. Blood Rev 12:91–98
Schulman S, Beyth RJ, Kearon C, Levine MN (2008) Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians evidence-based clinical practice guidelines (8th Edition). Chest 133:257S–298S. doi:10.1378/chest.08-0674
van der Meer FJ, Rosendaal FR, Vandenbroucke JP, Briet E (1993) Bleeding complications in oral anticoagulant therapy. An analysis of risk factors. Arch Intern Med 153:1557–1562
Leissinger CA, Blatt PM, Hoots WK, Ewenstein B (2008) Role of prothrombin complex concentrates in reversing warfarin anticoagulation: a review of the literature. Am J Hematol 83:137–143. doi: 10.1002/ajh.21046
Palareti G, Leali N, Coccheri S, Poggi M, Manotti C, D’Angelo A, Pengo V, Erba N, Moia M, Ciavarella N, Devoto G, Berrettini M, Musolesi S (1996) Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT). Italian Study on Complications of Oral Anticoagulant Therapy. The Lancet 348:423–428
Leendertse AJ, Egberts AC, Stoker LJ, van den Bemt PM (2008) Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med 168:1890–1896. doi: 10.1001/archinternmed.2008.3
Levi M (2009) Emergency reversal of antithrombotic treatment. Intern Emerg Med 4:137–145. doi: 10.1007/s11739-008-0201-8
Crowther MA, Ageno W, Garcia D, Wang L, Witt DM, Clark NP, Blostein MD, Kahn SR, Vesely SK, Schulman S, Kovacs MJ, Rodger MA, Wells P, Anderson D, Ginsberg J, Selby R, Siragusa S, Silingardi M, Dowd MB, Kearon C (2009) Oral vitamin K versus placebo to correct excessive anticoagulation in patients receiving warfarin: a randomized trial. Ann Intern Med 150:293–300
Keeling D, Baglin T, Tait C, Watson H, Perry D, Baglin C, Kitchen S, Makris M (2011) Guidelines on oral anticoagulation with warfarin—fourth edition. Br J Haematol 154:311–324. doi:10.1111/j.1365-2141
Lubetsky A, Yonath H, Olchovsky D, Loebstein R, Halkin H, Ezra D (2003) Comparison of oral versus intravenous phytonadione (vitamin K1) in patients with excessive anticoagulation: a prospective randomized controlled study. Arch Intern Med 163:2469–2473. doi:10.1001/archinte.163.20.2469
Crowther MA, Ageno W, Schnurr T, Manfredi E, Kinnon K, Garcia D, Douketis JD (2005) Oral vitamin K produces a normal INR within 24 h of its administration in most patients discontinuing warfarin. Haematologica 90:137–139
Makris M, Watson HG (2001) The management of coumarin-induced over-anticoagulation Annotation. Br J Haematol 114:271–280
Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G (2012) Oral anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141:e44S–e88S. doi:10.1378/chest.11-2292
Bechtel BF, Nunez TC, Lyon JA, Cotton BA, Barrett TW (2011) Treatments for reversing warfarin anticoagulation in patients with acute intracranial hemorrhage: a structured literature review. Int. J Emerg Med 4:40. doi:10.1186/1865-1380-4-40
Demeyere R, Gillardin S, Arnout J, Strengers PF (2010) Comparison of fresh frozen plasma and prothrombin complex concentrate for the reversal of oral anticoagulants in patients undergoing cardiopulmonary bypass surgery: a randomized study. Vox Sang 99:251–260. doi:10.1111/j.1423-0410.2010.01339.x
Yang L, Stanworth S, Hopewell S, Doree C, Murphy M (2012) Is fresh-frozen plasma clinically effective? An update of a systematic review of randomized controlled trials. Transfusion 52:1673–1686. doi:10.1111/j.1537-2995.2011.03515.x
Holland L, Warkentin TE, Refaai M, Crowther MA, Johnston MA, Sarode R (2009) Suboptimal effect of a three-factor prothrombin complex concentrate (Profilnine-SD) in correcting supratherapeutic international normalized ratio due to warfarin overdose. Transfusion 49:1171–1177. doi:10.1111/j.1537-2995.2008.02080.x
Vigue B (2009) Bench-to-bedside review: optimising emergency reversal of vitamin K antagonists in severe haemorrhage—from theory to practice. Crit Care 13:209. doi:10.1186/cc7701
Franchini M, Lippi G (2010) Prothrombin complex concentrates: an update. Blood Transfus 8:149–154
Baker RI, Coughlin PB, Gallus AS, Harper PL, Salem HH, Wood EM (2004) Warfarin reversal: consensus guidelines, on behalf of the Australasian Society of Thrombosis and Haemostasis. Med J Aust 181:492–497
Dentali F, Marchesi C, Pierfranceschi MG, Crowther M, Garcia D, Hylek E, Witt DM, Clark NP, Squizzato A, Imberti D, Ageno W (2011) Safety of prothrombin complex concentrates for rapid anticoagulation reversal of vitamin K antagonists. A meta-analysis. Thromb Haemost 106:429–438. doi:10.1160/TH11-01-0052
Sorensen B, Johansen P, Nielsen GL, Sorensen JC, Ingerslev J (2003) Reversal of the International Normalized Ratio with recombinant activated factor VII in central nervous system bleeding during warfarin thromboprophylaxis: clinical and biochemical aspects. Blood Coagul Fibrinolysis 14:469–477
Chai-Adisaksopha C, Hillis C, Siegal DM, Movilla R, Heddle N, Iorio A, Crowther M (2016) Prothrombin complex concentrates versus fresh frozen plasma for warfarin reversal. A systematic review and meta-analysis. Thromb Haemost 116:879–890. doi:10.1160/th16-04-0266
Voils S, Baird B (2012) Systematic review: 3-factor versus 4-factor prothrombin complex concentrate for warfarin reversal: does it matter? Thromb Res 130:833–840. doi:10.1016/j.thromres.2012.10.001
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012. doi:10.1016/j.jclinepi.2009.06.005
Johansen M, Wikkelso A, Lunde J, Wetterslev J, Afshari A (2015) Prothrombin complex concentrate for reversal of vitamin K antagonist treatment in bleeding and non-bleeding patients. Cochrane Database Syst Rev 7:Cd010555. doi:10.1002/14651858.CD010555.pub2
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. doi:10.1136/bmj.d5928
Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, Niu Y, Du L (2015) The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med 8:2–10. doi:10.1111/jebm.12141
Desmettre T, Dehours E, Samama CM, Jhundoo S, Pujeau F, Guillaudin C, Hecquart C, Clerson P, Crave JC, Jaussaud R (2012) Reversal of Vitamin K Antagonist (VKA) effect in patients with severe bleeding: a French multicenter observational study (Optiplex) assessing the use of Prothrombin Complex Concentrate (PCC) in current clinical practice. Crit Care 16:R185. doi:10.1186/cc11669
Desmettre T, Dubart AE, Capellier G, Fanara B, Puyraveau M, Kepka S, Coquart J, Sheppard F, Tazarourte K (2012) Emergency reversal of anticoagulation: the real use of prothrombin complex concentrates: a prospective multicenter two year French study from 2006 to 2008. Thromb Res 130:e178–e183. doi:10.1016/j.thromres.2012.05.029
Dowlatshahi D, Butcher KS, Asdaghi N, Nahirniak S, Bernbaum ML, Giulivi A, Wasserman JK, Poon MC, Coutts SB (2012) Poor prognosis in warfarin-associated intracranial hemorrhage despite anticoagulation reversal. Stroke 43:1812–1817
Evans G, Luddington R, Baglin T (2001) Beriplex P/N reverses severe warfarin-induced overanticoagulation immediately and completely in patients presenting with major bleeding. Br J Haematol 115:998–1001
Huhtakangas J, Tetri S, Juvela S, Saloheimo P, Bode MK, Karttunen V, Karajamaki A, Hillbom M (2012) Improved survival of patients with warfarin-associated intracerebral haemorrhage: a retrospective longitudinal population-based study. Int J Stroke 10:876–881. doi:10.1111/j.1747-4949.2012.00926.x
Kalina M, Tinkoff G, Gbadebo A, Veneri P, Fulda G (2008) A protocol for the rapid normalization of INR in trauma patients with intracranial hemorrhage on prescribed warfarin therapy. Am Surg 74:858–861
Karaca MA, Erbil B, Ozmen MM (2014) Use and effectiveness of prothrombin complex concentrates versus fresh frozen plasma in gastrointestinal hemorrhage due to warfarin usage in the ED. Am J Emerg Med 32:660–664. doi:10.1016/j.ajem.2014.02.016
Kuwashiro T, Yasaka M, Itabashi R, Nakagaki H, Miyashita F, Naritomi H, Minematsu K (2011) Effect of prothrombin complex concentrate on hematoma enlargement and clinical outcome in patients with anticoagulant-associated intracerebral hemorrhage. Cerebrovasc Dis 31:170–176. doi:10.1159/000321766
Leal-Noval SR, Lopez-Irizo R, Bautista-Paloma J, Casado M, Arellano-Orden V, Leal-Romero M, Fernandez-Hinojosa E, Puppo-Moreno A, Munoz M (2013) Efficacy of the prothrombin complex concentrate prothromplex in patients requiring urgent reversal of vitamin K antagonists or presenting with uncontrolled bleeding: a retrospective, single center study. Blood Coagul Fibrinolysis 24:862–868. doi:10.1097/MBC.0b013e3283650cf9
Lubetsky A, Hoffman R, Zimlichman R, Eldor A, Zvi J, Kostenko V, Brenner B (2004) Efficacy and safety of a prothrombin complex concentrate (Octaplex) for rapid reversal of oral anticoagulation. Thromb Res 113:371–378. doi:10.1016/j.thromres.2004.04.004
Majeed A, Eelde A, Agren A, Schulman S, Holmstrom M (2012) Thromboembolic safety and efficacy of prothrombin complex concentrates in the emergency reversal of warfarin coagulopathy. Thromb Res 129:146–151. doi:10.1016/j.thromres.2011.07.024
Majeed A, Meijer K, Larrazabal R, Arnberg F, Luijckx GJ, Roberts RS, Schulman S (2014) Mortality in vitamin K antagonist-related intracerebral bleeding treated with plasma or 4-factor prothrombin complex concentrate. Thromb Haemost 111:233–239. doi:10.1160/th13-07-0536
Pabinger I, Brenner B, Kalina U, Knaub S, Nagy A, Ostermann H (2008) Prothrombin complex concentrate (Beriplex P/N) for emergency anticoagulation reversal: a prospective multinational clinical trial. J Thromb Haemost 6:622–631
Sarode R, Milling TJ, Refaai M, Mangione A, Schneider A, Durn BL, Goldstein JN (2013) Efficacy and safety of a 4-factor prothrombin complex concentrate in patients on vitamin K antagonists presenting with major bleeding: a randomized, plasma-controlled, phase IIIb study. Circulation 128:1234–1243
Tazarourte K, Riou B, Tremey B, Samama CM, Vicaut E, Vigue B (2014) Guideline-concordant administration of prothrombin complex concentrate and vitamin K is associated with decreased mortality in patients with severe bleeding under vitamin K antagonist treatment (EPAHK study). Crit Care 18:R81. doi:10.1186/cc13843
Varga C, Al-Touri S, Papadoukakis S, Caplan S, Kahn S, Blostein M (2013) The effectiveness and safety of fixed low-dose prothrombin complex concentrates in patients requiring urgent reversal of warfarin. Transfusion 53:1451–1458. doi:10.1111/j.1537-2995.2012.03924.x
Yanamadala V, Walcott BP, Fecci PE, Rozman P, Kumar JI, Nahed BV, Swearingen B (2014) Reversal of warfarin associated coagulopathy with 4-factor prothrombin complex concentrate in traumatic brain injury and intracranial hemorrhage. J Clin Neurosci 21:1881–1884. doi:10.1016/j.jocn.2014.05.001
Yasaka M, Sakata T, Minematsu K, Naritomi H (2002) Correction of INR by prothrombin complex concentrate and vitamin K in patients with warfarin related hemorrhagic complication. Thromb Res 108:25–30. doi:10.1016/S0049-3848(02)00402-4;10.1016/S0049-3848(02)00402-4
Soyuncu S, Aslan S, Mutlu H, Bektas F (2015) Prothrombin complex concentrates utility for warfarin-associated hemorrhage. Int J Clin Exp Med 8:2778–2783
Joseph R, Burner J, Yates S, Strickland A, Tharpe W, Sarode R (2015) Thromboembolic outcomes after use of a four-factor prothrombin complex concentrate for vitamin K antagonist reversal in a real-world setting. Transfusion 56:799–807. doi:10.1111/trf.13406
Author Contributions
MPAB and MC were responsible for conception and design. MPAB, KvG and JGD were responsible for analysis and interpretation of data, and drafting of the manuscript. All authors contributed to drafting of the manuscript or revising it critically for important intellectual content and provided final approval of the manuscript submitted.
Funding
This study was performed without financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.P.A. Brekelmans has nothing to disclose. K. van Ginkel has nothing to disclose. J.G. Daams has nothing to disclose. B.A. Hutten has nothing to disclose. S. Middeldorp reports Grant or Research Support from GSK/Aspen, BMS/Pfizer, Sanquin and Bayer, Consultant fees from Bayer, BMS/Pfizer, Boehringer Ingelheim and Daiichi Sankyo, Paid Instructor at Bayer, GSK BMS/Pfizer, Boehringer Ingelheim and Daiichi Sankyo outside the submitted work. M. Coppens has received consultancy and lecturing fees, as well as research support from Daiichi-Sankyo, Boehringer-Ingelheim, Bayer, Bristol Myers-Squibb, Pfizer and Sanquin Blood Supply outside the submitted work.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Brekelmans, M.P.A., Ginkel, K.v., Daams, J.G. et al. Benefits and harms of 4-factor prothrombin complex concentrate for reversal of vitamin K antagonist associated bleeding: a systematic review and meta-analysis. J Thromb Thrombolysis 44, 118–129 (2017). https://doi.org/10.1007/s11239-017-1506-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-017-1506-0